03 Mar 2022
03 Mar 2022
The Covid-19 Delta Variant: What You Need to Know
With widespread vaccination and SOPs in place, many of us were starting to relax about the pandemic. However, when news about the Delta variant—a highly contagious SARSCoV-2 virus strain was announced, it sent many of us back into fear mode. Dr. Baljinder Singh, Head of the Emergency Department clarifies the facts about this variant and how we can take precaution.

Overview
Delta is described by The Centers for Disease Control and Prevention (CDC) as more transmissible than the common cold and influenza, in addition to the viruses that trigger MERS, SARS, and Ebola. Dr. Singh explains, “Delta is the name given to the COVID-19 variant that was first detected in India in December 2020. It is believed to be 50 to 60 percent more infectious than the original and Alpha strain, as per British Authorities.”
Symptoms
According to Dr. Singh, the Delta variant may have slightly different symptoms as compared to the original strain and the Alpha variant because people may have antibodies from a previous infection or vaccination and due to the mutation of the virus. “This variant has proven to be more easily transmissible,” he says, and in fact, the Deltavariant COVID -19 has more of the common-cold like symptoms, including sorethroat, sneezing, and fever, but cough and loss of smell are not that common. A headache and runny nose are common, he tells, and people may think they have a common cold with headache and not COVID, thereby unknowingly spreading the infection. Other symptoms include hearing impairment, gastrointestinal symptoms like nausea, vomiting and diarrhea and blood clots.
The problem
The Delta variant is more worrisome because the viral load is around one thousand times higher than previous variants as per a Chinese study, points out Dr. Singh. “There is around 35 percent increase in hospitalizations due to the Delta variant in the US as per the CDC and the majority of the hospitalizations and COVID-19 related deaths are occurring in the unvaccinated people.” Protection from COVID-19 infection is the same and includes following proper hand hygiene, wearing masks in crowded spaces, and keeping safe distances. Seeking medical advice if any symptoms arise and to go for full vaccination as per your local medical guidelines.
Screening and treatment
There is no special test for the Delta variant and the COVID PCR test is still used to test, he says, but the positive COVID PCR tests can undergo genetic analysis that can confirm if it is the Delta variant.
The treatment is the same regardless of the infectious variant. “Mild to moderate infections are managed at home with symptomatic treatment and severe infections require hospitalization,” he says, with certain antivirals and monoclonal antibody medications administered for moderate to severe infections along with corticosteroids, anti thrombotics, high-flow oxygen, and ventilation. H
BY: Web Team
Magazine
COMMENTS: No Comments
 03 Mar 2022
03 Mar 2022
Prediabetes Is on the Rise in the UAE
While prediabetes is not high enough to be considered type 2 diabetes, unless some immediate lifestyle changes are made, it likely will develop into type 2 diabetes. HEALTH speaks with Dr. Ihsan Al Marzooqi, Emirati Digital Therapeutics entrepreneur to learn more.

Defined
According to Dr. Al Marzooqi, prediabetes is a serious health condition caused by the body not responding in the normal way to insulin produced by the pancreas. “Insulin is a naturally occurring hormone that lets blood sugar into cells to use as energy,” he says, and prediabetes usually occurs in people who have some insulin resistance or whose cells aren’t making enough insulin to keep blood glucose within the normal range. A prediabetic patient’s blood sugar levels are higher than normal, but not yet high enough to be diagnosed with type 2 diabetes. He adds, “Eventually, without enough insulin, the extra glucose stays in the bloodstream and over time can develop into type 2 diabetes.”
In the UAE
With no clear symptoms in the early stages, he points out that prediabetes can go years without ever being detected and it’s currently affecting around 1.2 M people in the Emirates. “Prediabetes is rising in the region and the number of people impacted is alarming,” he tells, and this silent health crisis is affecting almost 15 percent of the UAE’s population; it’s most prevalent among UAE nationals, with around 19 percent of Emiratis and 15 percent of expatriates living with the condition.
Risk factors
Individuals over age 30, who are overweight, have a relative with type 2 diabetes, have a family history of hypertension, cardiovascular disease, or elevated blood fats and who are physically active less than three times a week, are those who are most at risk and should be screened as per the UAE guidelines, explains Dr. Al Marzooqi. “In some cases, the disease only reveals itself and its long-term implications when patients’ need urgent medical attention.
Dangerous repercussions
Those unaware they are living with it could be leaving it too late to treat and end up with a life changing chronic condition and serious and long-lasting health problems, he says, warning the community that prediabetes almost always leads to type 2 diabetes and those with the condition are at increased risk of heart disease and stroke if it continues to be untreated. Prediabetes shows very little symptoms until it is in its advanced stages; therefore, it’s recommended that those who are most at risk should get tested.
The good news
The good news, he tells, is that prediabetes is reversible, type 2 diabetes is not, although it can go into remission, so proactivity in the treatment of this condition is critical. “There are two ways of testing, first is to do an informal assessment of risk factors, usually best for asymptomatic adults, or the second option is to do a blood test,” he explains. “The key to reversing prediabetes is really all about education on the lifestyle choices that are needed and increasing awareness about how the foods we eat and the levels of physical activity we partake in, can dramatically impact our health.” H
BY: Web Team
Magazine
COMMENTS: No Comments
 02 Mar 2022
02 Mar 2022
Staying Breast Aware
With October being officially recognized as ‘Breast Cancer Awareness’ month, HEALTH speaks with consultant breast surgeon Dr. Rita Daaboul to learn more about the disease and how women can make themselves more breast aware.

Very early signs
The earliest signs of possible breast cancer are only picked up on screening tests, explains Dr. Daaboul. “These include microcalcification changes on a mammogram, or a small growth seen on a mammogram, or breast ultrasound which may as yet be too small to detect by touch.”
Self-breast exam and why it matters
According to Dr. Daaboul, it is recommended that every woman should self-examine her own breasts at least once every two months, preferably after her menstrual period, as that is the time when the breasts are the least lumpy and the least tender. She elaborates, “The idea is that over time, the woman would learn what her breasts normally feel like, so that if ever there is any change from the normal, she can recognize this early and seek a consultation with a breast surgeon for further professional assessment, as soon as possible.”
To check the breasts, the woman should look at her breasts in the mirror and then feel her breasts for lumps. “When checking the breasts in the mirror, she should look for any changes in the size or shape of the breasts, any dimpling or puckering or any skin changes, and also anything that may be different about the nipples,” she tells, and she should then feel her breasts at first standing up, and then lying down, especially if there are any concerns. She advises that the woman should use her flattened fingers to feel each part of the breast. This can be done in circles, all around the breast, in clockwise fashion, and lastly to feel the central area of the nipple.
Risk factors
In terms of age, Dr. Daaboul points out that the older a woman gets, the riskier it is to develop breast cancer. “The incidence of breast cancer is 1 in 8 women over their lifetime,” she says, while worldwide, the riskiest age is between 50 and 70 years of age. However, in the UAE, younger women tend to develop more advanced breast cancer, for an as yet unknown reason. As such, she recommends screening should begin earlier than in Western nations. “A woman is recommended to start mammographic screening from 40 years of age, and for a mammogram to be performed every 2 years.”
The latest treatment modalities
The most common treatment for breast cancer, reveals Dr. Daaboul, in simplified terms, is a combination of treatments which include surgery, chemotherapy, radiotherapy, hormonal treatment, and other biological treatments. “This is why breast cancer is treated by multiple specialists that discuss cases together and treat the patients’ in what is called a multidisciplinary team,” she says.
Lifestyle tips for women
While everyone has a certain degree of susceptibility to breast cancer, there are some straightforward lifestyle factors we can all undertake to lessen and avoid the risks, including:
Diet
Eat a healthy diet, rich in vegetables, fruit and natural, high-fiber whole foods. Avoid bad fats, red meat, and highly processed and junk foods.
Weight
Maintain healthy weight, especially as you approach old age.
Chemicals
Avoid toxic chemicals both at home and work.
Exercise and activity
Undertaking a regular exercise regime will certainly benefit overall health. Studies show that moderate weekly physical activity reduces the risk of breast cancer by around 20 percent.
Adequate vitamin D and sun
exposure.
Early pregnancy and breastfeeding is a proven preventative.
Mental health
Maintain a positive outlook which is proven to boost the immune system and works in both prevention and in better outcomes in those who are fighting cancer. H
BY: Web Team
Magazine
COMMENTS: No Comments
 23 Feb 2022
23 Feb 2022
Taking a Holistic Approach to Polycystic Ovarian Syndrome
With the influx of additives, hormones, and chemicals hidden in our food along with a sedentary lifestyle, polycystic ovarian syndrome is now becoming increasingly common, even in younger women. For a different approach, Khadija Kapasi, clinical dietitian/lifestyle expert instead focuses on mind-body medicine and lifestyle to manage PCOS.

PCOS defined
Polycystic ovary syndrome (PCOS) is a common condition that affects how a woman’s ovaries work, explains Kapasi. She elaborates, “If you have at least two of the following symptoms, you may be diagnosed with PCOS: irregular periods – which means your ovaries do not regularly release eggs (ovulation).” Also, excess androgen (male hormones) which is high levels of male hormones in your body, which may cause physical signs such as excess facial or body hair. “Or polycystic ovaries, when the ovaries become enlarged and contain many fluid-filled sacs (follicles) that surround the eggs,” she explains.
The approach
Maintain a healthy weight: maintaining a healthy weight can help decrease insulin resistance, regulate your period, and reduce your risk of conditions associated with PCOS. If you’re lean then weight gain or meeting the ideal body weight will be helpful here.
Balance your exercise
Exercise is important for maintaining a healthy weight, says Kapasi. “But too much exercise can disrupt your hormones; best are gentle, low impact exercises like yoga or Pilates which can be practiced for longer durations.” Swimming and light aerobics are also recommended.
Practice good sleep hygiene
Sleep affects your stress levels and helps regulate cortisol to balance your hormones, tells Kapasi. “But sleep disturbances are twice as common for women with PCOS.” To up your sleep hygiene, she advises to aim for 8 to 10 hours of sleep per night, establish a regular bedtime routine, avoid stimulants and rich, fatty foods before bedtime.
Reduce stress
Reducing stress can regulate cortisol. “Many of the aforementioned strategies mentioned above, such as yoga, getting enough sleep, and cutting caffeine, can contribute to lower stress levels,” she advises. “Taking walks outside and creating space in your life for relaxation and self-care can also reduce levels of personal stress.”
Limit or avoid endocrine disruptors
Endocrine disruptors are chemicals or ingredients that interfere with or block your body’s natural hormonal reactions. Some endocrine disruptors mimic female and male sex hormones, confusing your reproductive system. This, she says, can increase your risk of PCOS symptoms. They’re often found in canned foods, soaps, and makeup. Common endocrine disruptors include: dioxins, phthalates, pesticides, BPA, and glycol ethers. H
A holistic approach
Contraceptive pills and diabetes medications (which combat insulin resistance, a PCOS symptom) can help rectify the hormone imbalance and improve symptoms, reveals Kapasi. She prefers to understand the root cause of the condition with the help of a qualified professional and treat it accordingly. “What we need to ensure is that we have the four verticals of health kept together as they are interrelated and can nourish and flourish women’s health,” she tells. These are your diet, exercise, sleep, and mental health. A good balance of these four verticals can help regulate the hormones and menstrual cycle.
BY: Web Team
Magazine
COMMENTS: No Comments
 23 Feb 2022
23 Feb 2022
Stress and Your Digestion:a Closer Look at Peptic Ulcers
From work challenges to a stuck relationship, when stress and anxiety hit an all-time high and are not addressed in time the right way, it can trickle down into our digestive system, resulting in an ulcer. The good news is that it can be easily treated with medication and lifestyle modification. As HEALTH investigates.

What it is
According to Dr. Thomas James, Gastroenterologist, a peptic ulcer is erosion in the mucosa lining due to an increase in stomach acid. Basically, the lining of your stomach and first part of your small intestine, known as duodenum, have a layer of mucus that protects them from the acid which is produced by your stomach to help you digest food.
Different types
There are two different categories of peptic ulcers, he explains, one is duodenal and the other is gastric classified according to its location in the body. “The duodenal ulcer is found in the first part of the small intestine of the stomach and a gastric ulcer is located in the mucous membrane of the stomach.” While duodenal ulcer is more common, both are triggered by food, stress, and lifestyle.
Symptoms
The most common symptom, says Dr. James, is an aching of pain in the upper abdomen, a feeling of indigestion, hunger like pain, and vomiting. While the symptoms are the same for both types of ulcers, a key difference is the burning pain accompanying a duodenal ulcer which is caused by an empty stomach while gastric ulcer patients instead exhibit pain after eating.
Causes
An ulcer, he elaborates, is essentially caused by an increase in acid production which may be exacerbated by several factors. He adds, “One is Helicobacter pylori (H pylori) infection which is responsible for 60 percent of gastric ulcers and 90 percent of duodenal ulcers.” While H pylori is a bacterium that is commonly found in the stomach, the vast majority of people infected have no symptoms and will never develop problems. However, H pylori is capable of causing a number of digestive problems, including ulcers. Usually an ulcer will take a few months to heal, but may recur from habits, says Dr. James. “Overall lifestyle modification is the most important form of prevention and treatment also.”
Specific treatment
Acid secretion can be helped by diet modification, consuming meals on time, smoking cessation, and especially stress modification. With regards to medication, he explains that powerful proton pump inhibitors known as PPI are now being used effectively to provide short-term (two to eight weeks) treatment for ulcers in the stomach and in the upper small intestine, which can block more than 90 percent of stomach acid production. Also, treatment of H Pylori infection usually leads to clearing of infection, relief of symptoms, and eventual healing of ulcers. “Recurrence of infection can occur and retreatment may be required, if necessary with other antibiotics,” he says, but the treatment is targeted at eradicating the bacterial infection; the ulcer then heals and relapses are prevented.
Work on stress
Get a good amount of sleep: A proper amount of sleep helps relax and recuperate the mind and body, with the rest helping to reduce some of the ill-effects of stress.
Exercise
Exercising helps keep the body fit and helps release endorphins that could potentially help mitigate some of the more physical and even mental effects of stress.
Maintain a strong social network
Having a strong network of support and care can also help when feeling stressed.
Cultivate a positive mindset
Having a positive mind-set makes tackling stress easier than doing so with a pessimistic attitude.
Write a fun list
Take time out to write down a list of things that you love doing. Then when you are feeling down, you can consult your list and depending on how much time you can manage, put something that you love doing into the day. H
(Credit: www.experiencelife.com)
BY: Web Team
Magazine
COMMENTS: No Comments
 22 Feb 2022
22 Feb 2022
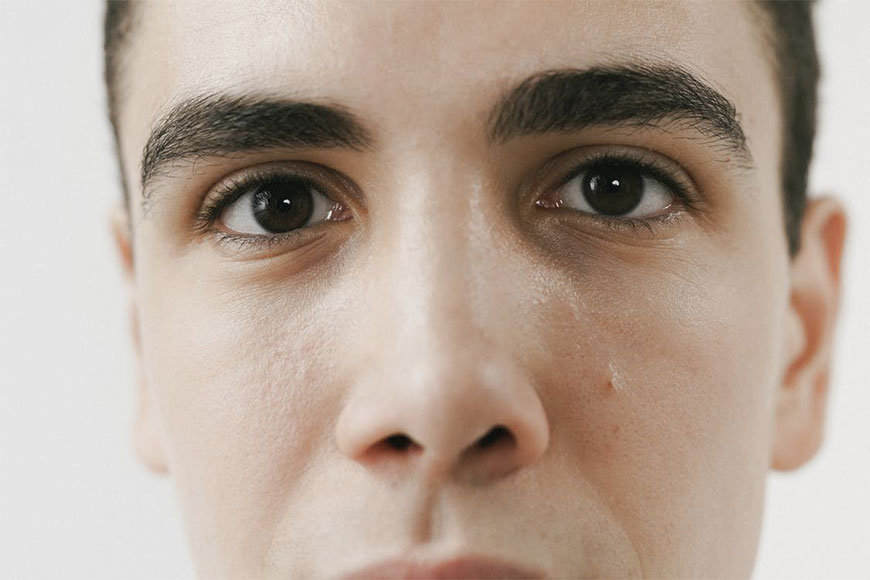
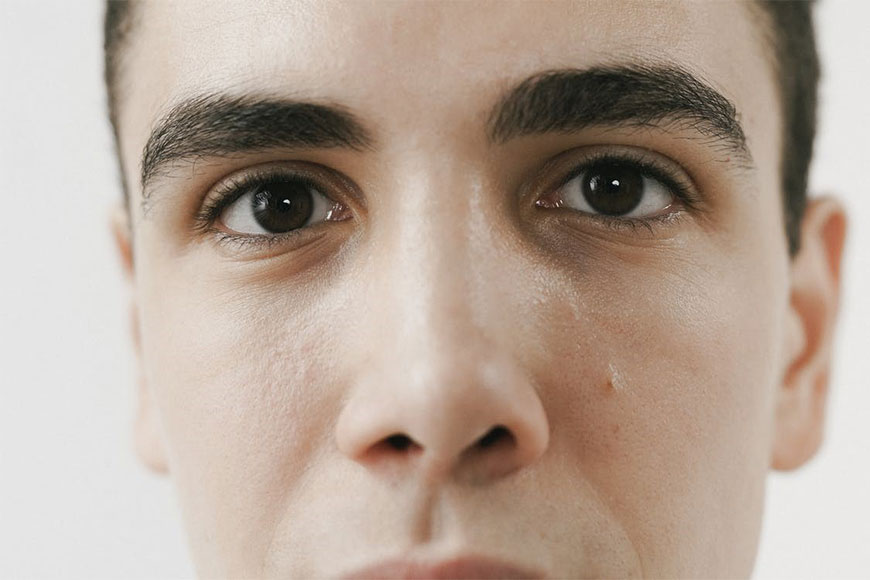
What Makes Male Depression Different
There is a stereotype of what depression looks like. We believe it has to be lots of crying, feelings of worthlessness, reduced appetite, excessive sleeping, isolating and being low all the time. To clarify, Jyotika Aggarwal, DHA Licensed Clinical Psychologist in Dubai discusses the red flags of male depression.

Facts versus stereotypes
According to Aggarwal, there is a stereotype of what depression looks like. “We believe it has to be lots of crying, feelings of worthlessness, reduced appetite, excessive sleeping, isolating and being low all the time.” While these are true and an important part of depression, for men, she explains that depression can look very different and this is the very reason why it may often be missed. She elaborates, “In men, it may manifest with symptoms like increase in fatigue, increased irritability and anger, sometimes they may become abusive in nature, loss of interest in work or hobbies, and difficulty in falling asleep.” Research also suggests that men use more substances, possibly as a form of self-medication. This can hide the symptoms of depression, making it harder to detect and treat effectively.
Less likely to reach out and seek help
Research suggests that men are not likely to accept their symptoms as depression hence, less likely to accept or seek help, points out Aggarwal. “Men find it hard to admit that they are going through any sort of difficulty let alone mental health concerns,” she says, and men are usually uncomfortable with any sign of weakness within themselves and may be afraid of being judged as a lesser man. Culturally, men are also not taught how to respond to their feelings of negativity, discomfort, or feelings of being low. “They believe they don’t even need to learn and can figure out a way to deal with this.”
Societal and cultural expectations play a role
Society and cultural beliefs also play a large role in this, she suggests. “Men, from time immemorial are required to be ‘strong’, which in turn pushes them to suppress any emotions that make them vulnerable,” she says; they are told from childhood ‘boys don’t cry’, and as they grow older, they are told to ‘get over it’. A manly framework is culturally depicted by the elders, explains Aggarwal, and the men have to abide by it. “They get so stuck to this reality that the world has built for them, that they may lose sight of their own emotional difficulties,” she says. “Many cultures associate respect with being manly and those men, who seek help often or may show an emotional side, are often judged in a negative light and not seen as reliable.” Men greatly fear such rejection and judgment, thus making it harder for them to seek help for their depression and anxiety.
How depression impacts men
When depressed, men’s daily life and the way they process situations changes, she says. “It can interfere with their productivity, negatively impact their relationships, and have sudden changes in their eating and sleeping patterns,” she says, and they are likely to be more on the edge, snap faster, and feel more anger. They are internally upset with themselves for not feeling ‘normal’ and feeling emotional discomfort, hence any small incident or conversation can provoke them. “In trying to tackle this situation, men may start avoiding family situations, become workaholics, start controlling, and become abusive in relationships,” she tells.
Expert advice
Aggarwal points out that the most important thing to remember is we are all human. “We all need support and compassion sometimes and we must not let external, dogmatic thoughts rule us to a point, that it becomes harmful for us,” she says, reminding us that it’s important to open doors for healthy and meaningful actions which help a person live their best life. H
BY: Web Team
Magazine
COMMENTS: No Comments
 17 Feb 2022
17 Feb 2022
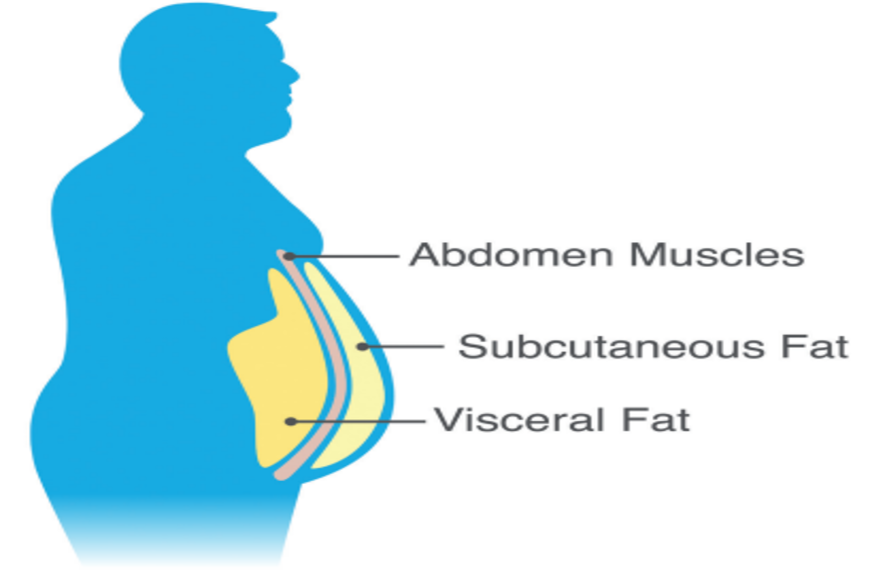
Shaking Up Your Visceral Fat Once and for All
Into the new year, many of us are making goals to lose weight. More specifically, visceral fat is not only dangerous, but it can trigger multiple health issues if not tackled in time. To learn more, HEALTH meets with Bryan Serrao, Personal Trainer at Body & Soul Health Club who provides the facts about this common problem.

What is visceral fat?
Visceral fat or belly fat, explains Serrao, is the fat within the abdominal cavity surrounding the internal organs. He elaborates, “Our bodies need some fat for its energy reserves, but our modern day lifestyles do not have the physical workload our bodies have been built to endure,” he says, and this in turn, leads to a surplus of fat especially around the tummy and thighs.
Why it matters
According to Serrao, scientific studies have shown that visceral fat is directly linked with heart disease, Alzheimer’s disease, type 2 diabetes, high blood pressure, and high cholesterol. It also raises the risk of stroke. He adds, “Researchers speculate that visceral fat creates an increase of certain proteins that inflame your body’s organs and tissues and ultimately narrow your blood vessels. In turn, this can trigger blood pressure to rise which can trigger other health issues.
How to measure it
A challenge about visceral fat is that there’s no way to ascertain how much visceral fat there is and where it’s concealed in the body without the use of highly specialized imaging tests. “The good news is these tests are rarely required and instead, there is a simple method to obtain an approximation,” says Serrao. “One is by the waist size; simply wrap a measuring tape around your waist over your belly button, ensuring you are not holding in your stomach.” In women, 35 inches or more is an indicator of visceral fat, while in men, it’s 40 inches. He warns that this method is quite rudimentary, especially if you’re a very large sized person. “And if you’re of Asian descent, the benchmark for visceral fat drops to 31.5 inches for women and 35.5 inches for men.”
Causes for the increase in visceral fat with aging
In simple words, Serrao points out that a calorie surplus diet is what causes visceral fat. “When the body is not burning the calories that are consumed, it stores the excess energy in the form of fat,” he says. “As our body ages, the metabolism rate—the rate at which food is converted into energy—gets slower and slower.” Age also plays a major role as there are hormonal changes which regulate important hormones. Also, stress is one of the underlying causes of excessive visceral fat. Stress causes the body to release a hormone known as cortisol, which increases how much visceral fat a person’s body stores, he explains.
The challenge in shedding visceral fat
There are two main types of fat, brown and white, explains Serrao. “Brown is considered as the good fat and is found in the front and back of the neck and upper back,” he says, while white fat is most prevalent in the body and has a number of roles that include temperature regulation, energy storage, protection of organs, and to protect the neuromuscular system. “Visceral fat falls in this category,” he says, and visceral fat is the most stubborn type of body fat as it is one of the last energy stores. The body is therefore programmed to hold onto visceral fat for as long as possible. “It is this reason that shedding this fat requires dedication, motivation, and patience as it needs to be defeated, not just burned.”
Exercises for visceral fat
Cardio, he explains, remains a popular choice. “However, just like diet, exercise also needs to be balanced and therefore, strength training/resistance/weight training should never be compromised,” he concludes. H
BY: Web Team
Magazine
COMMENTS: No Comments
 15 Feb 2022
15 Feb 2022
Eating an Anti-Cancerous Diet
A healthy lifestyle can reduce the risks of certain cancers and research indicates that many types of cancers are linked to unhealthy eating patterns and a sedentary lifestyle. Here to explain more, Dietician Fahmida Jafri reveals how to incorporate a diet that may just help reduce your risk of cancer.

What it means
To eat healthy and to avoid the risk of cancer, Jafri recommends that an individual should maintain a healthy weight within normal BMI range. “There should be more whole grains, fresh vegetables and fruits included in the diet as well as a reduction in sugary, processed foods,” she says, as well as the inclusion of plant proteins, healthy fats, and fiber rich foods in the daily diet.
Not limited to what we consume, she urges regular physical activity. “Keep yourself active; get involved in outdoor sports, walking, jogging or swimming at least three times a week, minimum one hour per session,” Jafri explains. “Also, the best lifestyle includes a good sleep cycle, no dependencies, less stress, and good rest.”
Specific foods
According to Jafri, non-starchy vegetables, whole fruits and whole grains are linked with a lower cancer risk. She elaborates, “It is believed that the pigments in vegetables and fruits are the most protective against cancer. So enjoy a variety of these foods as they are often rich sources of a variety of nutrients.” Fill half your plate with vegetables and fruits, and make at least half of your grains whole grains. Focus on the colorful fruits and vegetables such as eggplant, broccoli, kale, squash, oranges, kiwi, and so on, she says, to gain maximum benefits from their anti carcinogenic properties. “Many fruits and vegetables have cancer-fighting potential; for example, lycopene, a phytochemical found in cooked tomatoes and tomato products, has been shown to slow the growth of breast, lung, and endometrial tumors and to reduce prostate, stomach, and pancreatic cancer risks.”
The protein debate
Protein is the nutrient of importance for immunity and sustained health, she tells. “However, people recognize animal based protein with less importance given to plant proteins; both types have their own advantages.” To avoid inflammation and risk of cancers, it is strongly recommended to include plant proteins as 50 percent of your total protein intake. Research indicates a link between the consumption of red meat and processed meat to colon and other cancers, she says, so it is wise to choose lean meat over processed meats, reduce the portion size/frequency and importantly, include plantbased protein in the form of kidney beans, lentils, chickpeas, tofu, tempeh, and so on.
Good fats
The American Cancer Society says high saturated-fat diets are associated with an increased risk of colon, rectal, prostate, and endometrial cancers. They also state that the consumption of red meat has been linked to colon and prostate cancers. And gram for gram, fat has more than twice the calories of carbohydrates and protein, meaning excessive amounts is likely to cause weight gain. Instead, Jafri urges to consume fish two to three times a week in order to replace the high in saturated fat meat products. “Choose oils rich in MUFA, low-fat dairy and products free of trans-fats to avoid inflammation,” she notes, and include ground flaxseeds which contain soluble fiber, alpha linolenic acid (a form of healthy omega-3 fatty acid), and are the richest source of lignans (phytoestrogens that function like antioxidants).
Anti-cancerous diet checklist
- Strive to eat 10 servings (about half cup is a serving) of fruits and vegetables a day, choosing carotene-rich produce like carrots and cantaloupe, dark green vegetables, cruciferous vegetables, tomatoes, and citrus when possible.
- Broccoli, kale and Brussels sprouts contain sulphorane which a powerful antioxidant.
- Foods such as broccoli, berries, and garlic showed some of the strongest links to cancer prevention.
- Strawberries and raspberries are rich in antioxidants such as vitamin C and ellagic acid, a phytochemical.
- Spinach is rich in lutein and zeaxanthin, carotenoids that remove unstable molecules called free radicals from your body before they damage it. They’re found in spinach and other dark green leafy vegetables, and some studies show they could protect against cancer of the mouth, esophagus, and stomach. H
BY: Web Team
Magazine
COMMENTS: No Comments
 07 Feb 2022
07 Feb 2022
6 Care Tips for Rhinoplasty Aftercare
Rhinoplasty, aka a nose job, is a delicate procedure. Therefore, it’s necessary to take the aftercare seriously too. By being careful and taking a few necessary steps, the healing process is less likely to require an extended recovery time. Here are six care tips for rhinoplasty aftercare.
- Keeping Your Nose Clean
When cleaning your face, plan for it to require more time. Extra care must be taken to avoid putting unintended pressure on your nose during the healing process. Washing more slowly helps with this. Even when there is a partial nasal blockage, do not use your fingers to try to clear it. The nasal interior is very sensitive, especially after an operation, and damage could result. Cleaning the nose is a multi-step process to avoid damaging the tissues. Follow these carefully laid out nose cleaning tips after rhinoplasty to prevent a self-induced medical setback.
- Medicate the Pain
Depending on the surgeon, one or more pain medications will be administered or prescribed. Perhaps the most common is codeine; however, other medication will be provided if you’re allergic to it. Over-the-counter pain meds, such as Tylenol, are also useful too. Typically, the pain is increased a day or two post-surgery rather than immediately after it. However, this usually steadily decreases through the first week.
- Elevate the Head for Sleeping
Sleeping poses a particular risk for rhinoplasty surgeries. Rolling over must be prevented to avoid knocks to the nose. Sleeping on your back, even if this isn’t your usual sleeping posture, is best. Get a foam wedge or several pillows that encourage you to remain in the same position. An elevated head position is beneficial for the healing process too. If you doubt your ability to not roll over during sleep, using an armchair with a reclining feature is another option.
- Manage the Swelling
It’s natural to experience swelling during the recovery process. This can continue well into the second-month post-surgery. Use either an ice pack inside a soft towel or a cold compress to reduce the swelling. It’s helpful to do this at least five times a day, as needed. Do not apply pressure on the nose when using something to reduce inflammation though.
- Maintain a Balanced Diet
The recovery process requires protein, nutrients, and vitamins. These will help in the rebuilding process following the surgical procedure. Try to include some form of protein, eggs, fish, and nuts in your diet. If you’re either vegetarian or vegan, then choose the right alternatives for you. It’s also beneficial to ensure there are plenty of fresh greens in your recovery diet — broccoli, kale, or spinach are great for added vitamins.
- Avoid Exercise
It’s surprising how much everyday movement affects the nose and nasal cavities. Even stretching, bending to reach something from a lower shelf, or carrying shopping in from the car aggravates the nasal passages. All forms of exercise should be avoided for at least six weeks. Your doctor can provide advice on this timeline. Any jarring movement through exercise can cause inflammation during the healing process.
By following the above tips for self-care after getting a rhinoplasty, it encourages a smoother recovery period.
BY: Web Team
Magazine
COMMENTS: No Comments
 29 Jul 2021
29 Jul 2021
Cervical Cancer Screening

Prevention of cancer cervix:
The cervix is the bottom part of the uterus; it opens into the vagina
Cervical cancer happens when normal cells in the cervix change into abnormal cells and grow out of control.
There are two types of cervical cancer, “squamous cell carcinoma” and “adenocarcinoma.”
Cervical cancer screening tests:
Screening tests can find cervical cancer and precancer in the early stages when it can be treated, and thus may reduce the number of people who develop cervical cancer as well as the number of deaths due to the disease.
There are two types of screening test for cervical cancer:
- The Papanicolaou or “Pap” test (sometimes called a “Pap smear”)
- The human papillomavirus or “HPV” test
Or a Combination of both Tests
Risk Factors:
The most important risk factor for cervical cancer is infection with the human papillomavirus (HPV).
There are over 100 different types of HPV; however, most types of HPV do not cause cancer.
At least 80 percent of women are exposed to the HPV virus during their lifetime. Most of the time, the body’s immune system gets rid of the virus before it does harm.
HPV types are divided into high or low risk for causing cervical cancer.
- Low-risk HPV types – For example HPV types 6 and 11 can cause genital warts and are low-risk types because they rarely cause cervical cancer.
- High-risk HPV types – High-risk HPV types may cause cervical cancer in some people.
Although most people who are infected with the high-risk HPV types do not develop cervical cancer, those who repeatedly test positive for high-risk HPV are at a higher risk of cervical cancer.
HPV types 16 and 18 are two of the high-risk types.
How does HPV infection happen?
HPV is spread by direct skin-to-skin contact, including vaginal intercourse, oral sex, anal sex, or any other contact involving the genital area (eg, hand-to-genital contact).
So HPV is transmitted by sexual contact
Condoms provide only partial protection, since they do not cover all of the skin in the genital area.
It is not possible to become infected with HPV by touching an object, such as a toilet seat.
Course of HPV infection:
Most HPV infections are temporary and resolve within two years. People whose immune system cannot clear the virus (10-20%) are at higher risk of developing precancer or cancer. This usually takes many years.
Risk of cervical cancer increases in smokers, and those having a medical condition (or taking a medication) that weakens the immune system.
Symptoms:
Most people who are infected with HPV have no signs or symptoms.
How to reduce the risk of cervical cancer?
- A vaccine to help prevent infection with some high-risk types of HPV is recommended for all children ages 11 to 12 years, but it can be given as early as age 9. “Catch-up” vaccination is recommended for all people up to 26 years of age who have not yet received it, but it can be given up to age 45.
- Cervical cancer screening (even for those who are vaccinated)
- Smoking cessation
Cervical cancer screening
1-Pap test — The Pap test (sometimes called a “Pap smear”) is a method of examining cells from the cervix. Another term for a Pap test is “cervical cytology.”
For a Pap test, the provider will do a pelvic examination using a device called a speculum to open the vagina. Then they will use a small brush or spatula to collect cells from the cervix. This may be uncomfortable but usually is not painful. The cells are added to a container with preservative fluid or smeared on a glass slide for examination.
2-HPV test — Like a Pap test, the human papillomavirus (HPV) test is done during a pelvic examination, using a small brush to collect a sample from the cervix. HPV tests do not test for all different types of HPV. They only test for the strains of HPV that have a high risk for causing cervical cancer; a positive result indicates that one or more of these strains were found. Sometimes, the lab will specifically report if you have either of the two highest-risk HPV types, known as HPV 16 and HPV 18. This is called “genotyping.”
3-Combination test — This involves doing a Pap and HPV test at the same time; it is also called “co-testing.”
Screening tests can be done at any time during your menstrual cycle. However, not during the period.
Who should be screened?
The goal is to start screening at the point at which the benefits of screening are likely to outweigh the risks.
People who have received the vaccine should also be screened , since vaccines prevent the most common HPV infections but not all HPV infections.
Before age 21:
In healthy people, screening is not recommended
Age 21 to 29 —
- Screening can start in the age of 25 every 3 years with pap smear
Age 30 to 65
- HPV-only testing also called primary HPV testing) every five years if all results are normal
- “Co-testing” (both Pap and HPV testing) every five years
- A Pap test every three years if all results are normal
After age 65 — Most women with no risk factors can stop having cervical cancer screening after the age of 65
- Those who had all normal screening tests on a regular basis in the past.
- Those who have had at least three normal Pap tests in a row or two normal co-tests (combination Pap and HPV tests) over the past 10 years, with the most recent test within the past 5 years.
Some Womwn with Risk factors need to continue having cervical cancer screening beyond the age of 65 if:
- They had an abnormal Pap test, an abnormal HPV test, or treatment for cancer or precancerous cells of the cervix, vagina, vulva, or anus.
- They have HIV infection or another condition that suppresses the immune system.
- They were exposed to diethylstilbestrol (DES) the womb – DES is (a drug that was given to many women before 1981 to prevent pregnancy complications).
After hysterectomy (surgical removal of the uterus and sometimes the cervix
- If cervix was removed, no need for further screening.
- If cevix is not removed ( regular guidelines should be followed)
SCREENING TEST RESULTS
Pap test — If a Pap test was done as part of your cervical cancer screening, the results from your Pap test will be available a few weeks after your visit. Pap test results may be reported as:
- Negative– Pap tests that have no abnormal, precancerous, or cancerous cells are labeled as negative for intraepithelial lesion or malignancy.
- Abnormal results– Cervical cells may appear abnormal for a variety of reasons. For example, you may have a cervical infection or you may have a precancerous area or even cervical cancer.
HPV test — If a human papillomavirus (HPV) test was done as part of your cervical cancer screening, the results will be available a few weeks after your visit. The results may be reported as:
- Negative– There are no high-risk HPV strains present.
- Positive– There are high-risk HPV strains present. Some labs will specify if the highest-risk HPV types (HPV 16 or HPV 18) are present.
Follow-up testing — If your Pap or HPV test results are abnormal, you may need follow-up testing or colposcopy ( checking the cervix with a microscope) and taking biopsy-depending on the abnormality.
Finally:
Cervical cancer screening is easy and widely available and is the most important step in preventing cervical cancer and saving lives!
BY: Web Team
Magazine / Uncategorized
COMMENTS: No Comments