A common underdiagnosed disorder commonly found among the overweight, is caused by a repetitive collapse of the upper respiratory passage during sleep. This causes a partial or complete obstruction to breathing. The obstruction can occur at the level of the nose, nasopharynx, Oropharynx, hypopharynx, mandible or neck. An affected person presents with snoring, disturbed sleep with episodes of choking or gasping, daytime irritability, loss of concentration at work or school and morning fatigue due to excessive daytime sleepiness.
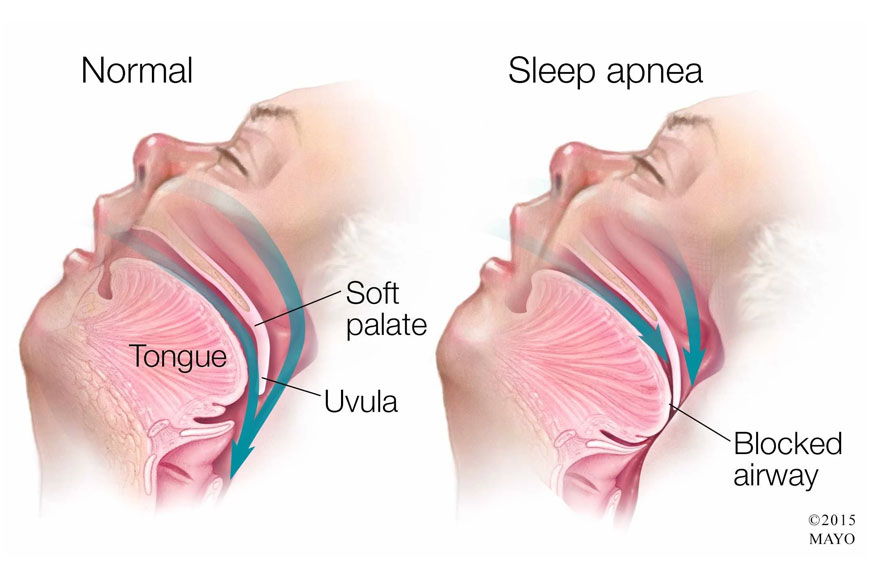
The periodic obstruction despite patients continued respiratory effort with disturbed sleep leads to low oxygen levels in the blood. Prolonged obstruction could lead to pulmonary or systemic hypertension, cardiac arrhythmias, congestive cardiac failure and other heart conditions like myocardial infarction etc. Memory loss, morning headaches, mood swings, depression are other problems an affected person would have to deal with. Increased sleepiness in the daytime is a leading cause of road accidents especially in long distance drivers. Hence snoring is no longer a facetious affair, it needs to be taken seriously and treated adequately.
For starters weight loss with diet and exercise support could help reduce the problem. An ENT specialist needs to do a complete clinical examination and Fibre-optic nasopharyngo-laryngoscopy to check the level of anatomic abnormality contributing to the sleep disordered breathing. Sleep study or Nocturnal polysomnography is recommended to confirm the presence and severity of the obstruction. The degree of hypoxemia, hypercapnia, inspiratory flow limitation and the number of arousal episodes are measured during the study. Recent modalities to assist in the diagnosis of OSA are – DISE ( Drug Induced Sleep Endoscopy is currently employed to assist in the diagnosis of the level of obstruction in the upper airway passage. It’s an endoscopy when the patient is put under deep anaesthesia by an anesthetist to locate and evaluate the site of obstruction. Functional MRI is also found to be useful to specify the area of narrowing causing a compromise in the upper airway.
Nasal CPAP remains the gold standard for obstructive sleep apnea. This consists of a Continuous Positive Airway Pressure therapy that’s just high enough to prevent collapse of the airway. The pressurized air is provided through a mask that seals around the mouth or nose. This allows the patient to breathe without much effort and without episodic awakening.
Site specific surgical therapy (Nasal/ Palatal / Hypo pharyngeal or Base of Tongue) or staged surgical management ( if obstruction is at more than one anatomical level in the upper respiratory tract) may be needed with improvement in the condition.
The new innovative treatment by the use of hypoglossal nerve stimulation via a small impulse generator implanted beneath the clavicle with a tunneled breathing sensing lead placed between the external and intercostal muscles, and a tunneled stimulation lead attached to the branch of the hypoglossal nerve that produces protrusion of tongue during inspiration via the genioglossus muscle has proved helpful in reducing the apneic episodes in affected patients.
Dr. Meenu Cherian
ENT Specialist
Thumbay University Hospital