11 Apr 2022
11 Apr 2022
Here is About Pneumonia
What is pneumonia?
Pneumonia is a contamination of one or the two lungs brought about by microbes, infections or organisms.
At the point when there is a disease in the lungs, a few things occur, including:
- Your airway swells (becomes inflamed)
- The air sacs in the lungs are filled with mucus and other fluids

How do the lungs work?
The main job of your lungs is to get oxygen into your blood and remove carbon dioxide. This happens during breathing. You breathe 12 to 20 times a minute when you’re not sick. The trachea is divided into airways (bronchial tubes). One of the bronchial tubes leads to the left lung and the other to the right lung. For the lungs to perform best, the airways must be open during inhalation and exhalation. Swelling (inflammation) and mucus can make it difficult to move air through the airways, making breathing more difficult. This leads to shortness of breath, difficulty breathing and feeling more tired than usual.
How common is pneumonia?
Nearly one million adults in the United States are hospitalized each year with pneumonia and 50,000 people die from the disease. This is the second most common reason for hospitalization – childbirth is the first. Pneumonia is the most common cause of hospitalization for children in the United States. Older adults who are hospitalized with pneumonia have a higher risk of death than any of the other 10 causes of hospitalization.
Is pneumonia contagious?
Certain types of pneumonia are contagious (passed from person to person). Pneumonia caused by bacteria or viruses can be contagious when disease-carrying organisms are inhaled into your lungs. However, not everyone who is exposed to the pneumonia-causing germs gets it.
Pneumonia caused by fungi is not contagious. The fungi are in the soil, airborne and inhaled, but they are not transmitted from person to person.
How pneumonia is communicated starting with one individual then onto the next?
Pneumonia is spread when droplets of fluid containing pneumonia bacteria or virus are released into the air when someone coughs or sneezes and then others inhale it. You can also get pneumonia from touching an object that a person with pneumonia has touched (the transmission of germs) or a tissue used by the infected person and then touching your mouth or nose.
How long will I be contagious if I have pneumonia?
If you have bacterial pneumonia, it is still considered contagious until about the second day after you start taking the antibiotics and you no longer has a fever (if you have one). If you have viral pneumonia, you will remain contagious until you feel better and have a fever for several days.
In adults, what are the signs and symptoms of bacterial versus viral pneumonia?
Indications of pneumonia can go from gentle (cold or influenza like manifestations) once in a while called “versatile pneumonia” to serious. The severity of your pneumonia depends on the specific germ causing the pneumonia, your general health, and your age.
Bacterial pneumonia: Symptoms of bacterial pneumonia can grow progressively or unexpectedly. Symptoms include:
- A high temperature (up to 105 degrees Fahrenheit)
- fatigue (tiredness)
- Difficulty breathing: fast breathing or windedness
- perspiring
- Goosebumps
- Mucus cough (may be greenish or contain a small amount of blood)
- Chest and/or abdominal pain, especially with coughing or deep breathing
- Anorexia
- Confused mental state or changes in consciousness (especially in older adults)
Viral pneumonia: Symptoms usually appear over several days. Early symptoms are similar to those of the flu, which include:
- Fever
- dry cough
- Headache
- sore throat
- Anorexia
- muscle pain
- weakness
Additional symptoms that appear after about a day include:
- high temperature
- coughing with mucus
- Shortness of breath
How can I tell if I have pneumonia versus a cold or the flu?
It’s hard to tell the difference but it’s important to know when to seek medical care
Pay attention to these persistent symptoms that occur in pneumonia:
- severe congestion or chest pain
- Breathing difficulties
- Fever of 102 or higher
- Cough that produces pus
Pneumonia symptoms last longer than cold and flu. If your symptoms are not severe, it is okay to try home remedies such as getting more rest, drinking more fluids, taking some over-the-counter medications and seeing what happens. But if you don’t notice an improvement in your symptoms after three to five days, or if you develop more serious symptoms such as dizziness or severe difficulty breathing, see your healthcare provider. do not let her go. Pneumonia; like symptoms in very young children or adults older than 65 are a cause for concern. Also, pneumonia can cause permanent lung damage if left untreated for a long time. And always seek immediate care if you have chest pain or difficulty breathing.
BY: Web Team
Magazine
COMMENTS: No Comments
 11 Apr 2022
11 Apr 2022
Here is about Rhinoplasty
Assuming you’re comfortable with the clinical term “rhinoplasty,” you’re mindful that the vast majority consider it rhinoplasty, a corrective strategy to change the look and feel of an individual’s nose. Around 300,000 rhinoplasty techniques are played out every year in the United States. People between the ages of 20 and 50 are most likely to undergo this procedure, and a gender balance is preferred by women, who have 59% of all surgeries.

However, rhinoplasty is not only about aesthetics. Although rhinoplasty is often chosen primarily to balance a person’s facial features, it can also treat structural problems that interfere with breathing, and it is also common for surgery to address both function and aesthetics.
The physiology of the nose is quite complex, and rhinoplasty is usually considered one of the most complex, requiring extensive knowledge of facial anatomy. However, it can be a remarkably effective procedure.
Deviated nasal septum
The septum is the cartilage flowing between the nostrils. It should be centrally located so that each air corridor is roughly the same size. The septum may be pushed to one side due to a broken nose or other injury, or you may be born with uneven passages.
If you are an active person, correcting a deviated nasal septum can improve airflow for effective cardiovascular performance. Rhinoplasty can reconstruct the structure of your nose to keep the septum in the middle.
Broken nose
Repairing damage from a broken nose is perhaps the most common non-cosmetic reason for rhinoplasty. It can include reshaping the cartilage or resetting the broken nasal bones.
Rhinoplasty for the after effects of a broken nose usually focuses on breathing function rather than increasing aesthetics. This is called corrective rhinoplasty.
Nose humps
A prominent hump on the bridge of your nose may give the impression that your nose has cracked, as unrepaired breaks can also create a hump. However, you may have excess cartilage that forms the hump without breaking your nose. Rhinoplasty can remove the excess, remove the hump, and reshape your nose.
Nose shape
Nose shape is a personal preference. Some people find their doorways to be too narrow, too wide, or unsatisfactory in some other respects. Rhinoplasty can correct the shape of the nose, but it is a surgical type of procedure, in which the entire physiology of the nose must be considered. Breathing function may affect how much your nose changes.
Big nose head
The exemplary protruding nose shape can toss the presence of your nose out of offset with the remainder of your face. As with nasal humps, the cartilage can be removed, and the common technique for adjusting the tip of the nose reaches the cartilage from the inside of the nose, so the scars from rhinoplasty are hidden from view.
Because of the complexity and potential differences with rhinoplasty surgery, an experienced surgeon is a must. Lakeshore ENT has a team of 16 surgeons who specialize in ear, nose and throat problems, including those who specialize in rhinoplasty. Whether you want to restore breathing function or rebalance the appearance of your face, call or click today to schedule a consultation.
It is critical to pick the right rhinoplasty specialist
While rhinoplasty is a typical corrective technique, numerous plastic specialists decide not to perform this is on the grounds that it presents many difficulties. In the nose, structure and capacity are firmly related. A cosmetic change in the structure of the nose may have undesirable effects on breathing. At the same time, specific surgical techniques designed to improve nasal breathing can affect the appearance – for better or worse.
As a result, a small percentage of surgeons perform a large percentage of rhinoplasty operations.
How much does rhinoplasty cost?
The response relies upon the reasons you need or need the medical procedure. The surgery is optional and not covered by insurance if it is done to correct the appearance of the nose. This may include reducing the bump on the bridge of your nose or modifying its shape or size.
Your insurance plan may cover a “functional” procedure if there is a medical condition, such as a stuffy nose, or if surgery is needed to correct breathing problems. If there are functional and appearance concerns, part of the procedure may be covered by insurance and part may not.
BY: Web Team
Magazine
COMMENTS: No Comments
 11 Apr 2022
11 Apr 2022
Here is about Tracheostomy
What is a Tracheostomy?
A tracheostomy is an opening (made through an incision) through the neck into the windpipe (windpipe). Opening the trachea opens the airway and helps breathing.
A tracheostomy can be performed in an emergency setting, at the patient’s bedside or in an operating room. Anesthesia (pain relief medicine) may be used before the procedure. Depending on a person’s condition, a tracheostomy may be temporary or permanent.

When is a tracheostomy considered?
A tracheostomy may be performed in the following cases:
- Mouth or throat blockage
- Difficulty breathing due to edema (swelling), injury, or lung (lung) disease
- Airway reconstruction after tracheostomy or laryngeal surgery
- Protect the airway from secretions or food due to swallowing problems
- Airway protection after head and neck surgery
- Long-term need for ventilator (respiratory) support
What is a tracheostomy tube?
A tracheostomy tube is a small tube that is inserted into a tracheostomy to keep the opening (opening) clean.
Tracheostomy tubes are available in many sizes and materials including semi-flexible plastic, rigid plastic, or metal. The tubes are disposable or can be reused. They may have an internal cannula that can be disposable or reused. The endotracheal tube may or may not have a cuff. Tracheostomy tubes are generally used for patients who have difficulty swallowing or who are receiving mechanical ventilation. Unconstrained endotracheal tubes are used to maintain a patient’s airway when a ventilator is not needed. The choice of tube depends on your condition, the shape and size of your neck, and the purpose of the tracheostomy.
All tracheostomy tubes have an external cannula (main shaft) and neck plate (flange). The lip on your neck is located above the opening (opening). The perforations on either side of the neck plate allow you to insert the tracheostomy tube ties to secure the tracheostomy tube in place.
After going home with a tracheostomy, what do I need to know?
Immediately after your tracheostomy, you will communicate with others by writing so that your health care provider can give you instructions on communication techniques.
Do not remove the external cannula unless your healthcare provider tells you to do so.
Use tracheostomy caps to protect your airway from outside elements (such as dust, cold air, etc.) Ask your healthcare provider for more information about tracheostomy caps and where to buy them.
When should I contact my healthcare provider?
- If you have an irregular heart rate
- If you feel increasing pain or discomfort
If you have trouble breathing and this is not cleared up in the usual way to filter secretions.
When the secretions become thick, if crusting occurs or mucous plugs are present. Your doctor may recommend increasing fluids or using cold mist humidification.
How do I take care of a tracheostomy tube?
Your nurse will teach you the correct way to care for your tracheostomy tube before you go home. Routine tracheostomy care should be done in some measure once per day after you are released from the medical clinic.
- Stand or sit comfortably in front of the mirror (the bathroom above the sink is a good place to take care of the tracheostomy tube).
- Put on gloves.
- Endotracheal puncture tube suction. (Your health care provider will give you more information about the aspiration procedure.)
- If your tube has an internal cannula, remove it. (If the endotracheal puncture tube does not have an internal cannula, go to step 12.)
- Hold the inner cannula over the sink and pour the hydrogen peroxide over it. Use as much hydrogen peroxide as you need to thoroughly clean the inner cannula.
- Clean the internal cannula with pipe cleaners or a little brush.
- Rinse the indoor cannula well with plain saline, tap water, or distilled water (if you have a septic tank or well water).
- Thoroughly dry the inside and outside of the indoor cannula with a clean 4″ x 4″ mesh gauze pad.
- Reinsert the internal cannula and lock it in place.
- Remove the soiled gauze pad around your neck and throw it away.
- Check the skin around the stoma for redness, hardness, tenderness, drainage, or a foul odor. If you notice any of these conditions, contact your nurse or doctor after you have completed routine care.
- Soak a cotton swab in a solution of half hydrogen peroxide and half water.
- Dampen the cloth with plain saline, tap water, or distilled water. Use the cloth to wipe the hydrogen peroxide and clean the leather.
- Dry the exposed external cannula and the skin around the stoma with a clean towel.
- Change the tracheostomy tube ties.
BY: Web Team
Magazine
COMMENTS: No Comments
 11 Apr 2022
11 Apr 2022
Who is a Neuro-Ophthalmologist?
Neuro-ophthalmologist
Having great visual perception makes it simpler to play out your everyday assignments. However, vision issues are a typical issue. In excess of 150 million Americans wear some type of remedial eyeglasses. The greater part: of grown-ups beyond 75 years old foster waterfalls. Glaucoma influences multiple million individuals beyond 40 years old. Multiple million Americans are outwardly weakened, and more than 1.3 million are legitimately visually impaired.

For most eye concerns or routine eye tests, you can visit an ophthalmologist or ophthalmologist. Ophthalmologists are specialists or orthopedists who represent considerable authority in diagnosing and treating eye infections. They get more preparation than optometrists and can along these lines treat a wide scope of issues.
A portion of these specialists have practical experience in explicit regions connected with vision. This incorporates neuro-ophthalmologists. Their area of expertise is vision issues brought about by neurological conditions.
How does a neuro-ophthalmologist respond?
Neuro-ophthalmology is a subspecialty of both nervous system science and ophthalmology. Neuro-ophthalmologists represent considerable authority in vision issues including your sensory system. These issues incorporate vision issues because of cerebrum injury or sickness, including injury, stroke, or contamination. Some of the time these issues may not be a not kidding goal for concern, yet different times, they can prompt more genuine entanglements, like vision misfortune.
A neuro-ophthalmologist can analyze and treat neurological and fundamental sicknesses that influence your vision and eye development. Tests they might give you incorporate electroretinography, optical lucidness tomography, and multifocal EGR accounts.
The treatment your neuro-ophthalmologists might give you relies upon your specific circumstance, however may include:
- remedial focal points
- Botox infusions for muscle fits
- surgeries
- Instruction and preparing of neuro-ophthalmologists
A neuro-ophthalmologist typically gets:
- Four year college education for quite some time
- long term clinical endorsement
- At least 5 years of clinical preparation after clinical school (residency and cooperation preparing)
Notwithstanding the schooling and preparing above, many (however not all) neuro-ophthalmologists have become bored affirmed in nervous system science, ophthalmology, or both. Board certificate implies that these specialists are fully informed regarding the most recent advancements in their field. Some get extra preparation to perform surgeries, while others might keep preparing to perform specific tests.
What conditions does Neuro-ophthalmologist treat?
Neuro-ophthalmologists analyze and treat various sorts of vision issues. A portion of the more normal conditions they treat include:
- twofold vision
- eyelid anomalies
- Miniature cranial nerve paralysis (at times called “diabetic nerve paralysis”)
- myasthenia gravis
- Optic nerve issues (optic neuritis, ischemic neuritis, Leber’s optic neuropathy)
- cerebral neuroma
- squint
- thyroid eye infection
Motivations to see a neuro-ophthalmologist
An ophthalmologist might allude you to a neuro-ophthalmologist on the off chance that you:
Lose visual sharpness
Loss of visual keenness (clearness and sharpness) may happen for an assortment of reasons, including uncorrected refractive mistakes, retinal issues, issues with the optic nerves, and issues inside your skull, like a cancer or aneurysm. A neuro-ophthalmologist can analyze the issue and suggest treatment choices.
You experience difficulty moving your eyes
Issues that keep your eyes from moving appropriately incorporate cranial nerve paralysis and myasthenia gravis. These issues make it difficult to see. You ought to likewise see a neuro-ophthalmologist assuming your eyes out of nowhere begin shaking, as this can be an indication of nystagmus, a condition that can create issues with vision, profundity discernment, equilibrium, and coordination.
You have cancers pushing on the optic pathways
Regardless of whether you notice any progressions in your vision, however have been determined to have a pituitary growth (or one more kind of cancer in your skull) pushing on your optic nerves, you should see a neuro-ophthalmologist to ensure you don’t have vision misfortune.
You have strain in your mind
Building strain in your mind can make your optic nerves swell, and in the end to lose your vision. It tends to be brought about by mind cancers and furthermore a condition called cerebral pseudotumor. A neuro-ophthalmologist can analyze and treat the reason.
Advancement of inconsistent understudies
Any unexpected changes in understudy size could show a difficult issue, like a mind aneurysm, and ought to be dealt with right away.
What do you anticipate from a nervous system specialist and ophthalmologist?
Before you go to a neuro-ophthalmology arrangement, you should ensure that you have:
- Your present glasses and remedies
- Related clinical records
- Duplicates of any MRI, CT examine, or other eye tests
BY: Web Team
Magazine
COMMENTS: No Comments
 11 Apr 2022
11 Apr 2022
What is laser treatment?
Laser therapy is the medical treatment that uses focused the light to stimulate a process called photobiomodulation, or PBM. During PBM, photons enter tissues and interact with the cytochrome c complex within the mitochondria. This interaction triggers a biological chain of events that increases cellular metabolism, reduces pain, reduces muscle spasm, and improves microcirculation to affected tissues. This treatment is the FDA approved and provides patients with a non-surgical, non-drug alternative to pain relief.

How does laser treatment work?
The laser treatment works by stimulating a process called photobiomodulation (PBM) in which photons enter tissues and interact with the cytochrome C complex within the mitochondria. To get the best therapeutic results from laser treatment, a sufficient amount of light should reach the target tissues. Factors that maximize target tissue reach include:
- Light wavelength
- Reduce reflections
- Reduce unwanted absorption
- Power
Treatment solutions
Laser therapy is used to treat acute and chronic conditions as well as recovery after activity. It is also used as another option for prescription medications, a tool to prolong the need for certain surgeries, as well as pre- and post-operative treatment to help control pain and swelling.
Acute conditions
Laser therapy has been shown to be effective to help treat severe cases. Getting the pain under control quickly aids the healing process and usually helps promote better outcomes.
Chronic diseases
In chronic cases, research has shown that therapeutic lasers can be used to help combat persistent pain and promote blood circulation to damaged tissue. It can be a powerful non-drug solution to help reduce pain without the side effects of medications.
Recovery after activity
LightForce® Therapy Lasers can be found on the sidelines of many professional, collegiate and Olympic sports teams across the United States and many parts of Europe and Asia. Laser therapy has been shown to be effective in improving recovery times after activity and reducing delayed onset muscle soreness (DOMS).
Class IV laser treatment
What is Class IV laser treatment? Effective administration of laser therapy is a direct function of the strength and time as it relates to the dose provided. Administration of the optimal treatment dose to patients produces consistent positive results. Class IV therapeutic lasers deliver more energy to deep structures in less time. This ultimately helps provide a dose of energy that leads to positive, repeatable results. The higher wattage also results in faster treatment times and provides changes in pain complaints that cannot be achieved with low-power lasers. The LightForce® laser offers a level of versatility unmatched by other Class I, II and IIIB lasers due to its ability to treat both superficial and deep tissue conditions.
Effectiveness
Laser treatment causes a series of therapeutic responses in your body. During the treatment, you will feel soothing warmth that marks the beginning of a process of altered cellular activity that leads to reduced pain and improved blood circulation in the treated area. Successful treatment programs require multiple treatments, and the number of weeks depends on the condition and severity of symptoms.
What is the purpose of laser treatment?
Laser therapy, or photobiomodulation, is a process where photons enter tissues and interact with the cytochrome c complex within the cell’s mitochondria. The result of this interaction, and the goal of laser therapy treatments, is the biological sequence of events that leads to an increase in cellular metabolism (promoting tissue healing) and a reduction in pain. Laser therapy is used to treat acute and chronic conditions as well as recovery after activity. It is also used as another option for prescription medications, a tool to prolong the need for certain surgeries, as well as pre- and post-operative treatment to help control pain.
Is laser treatment painful? How does laser treatment feel?
Laser treatments must be administered directly to the skin, because laser light cannot penetrate the layers of clothing. You will feel soothing warmth during treatment. Many patients receiving LightForce® Therapy Laser treatments have reported enjoying the experience, especially when the massage ball treatment head is used to deliver what is often referred to as “laser massage.”
Patients who frequently receive high-energy laser treatments also report a rapid reduction in pain. For someone with chronic pain, this effect can be especially pronounced. Laser treatment for pain can be a practical treatment.
Is laser treatment safe?
Class IV laser therapy devices (now called photodynamic bio modulation) were approved in 2004 by the FDA to safely and effectively reduce pain and increase microcirculation. Therapeutic lasers are safe and effective treatment options for reducing musculoskeletal pain caused by injury.
How long is the treatment session?
With the LightForce® laser, treatments are usually quick from 3 to 10 minutes depending on the size, depth and severity of the condition being treated. A high-powered laser is able to deliver a lot of energy in a small amount of time, allowing therapeutic doses to be obtained quickly. For patients and doctors with packed schedules, quick and effective treatments are a must.
How often will I need laser treatment?
Most doctors will encourage their patients to have 2-3 treatments per week when they start treatment. There is well-documented support that the benefits of laser treatment are cumulative, indicating that plans to incorporate lasers as part of a patient’s care plan should include early and frequent treatments that can be administered less frequently as symptoms resolve.
How many treatment sessions will I need?
The nature of the condition and the patient’s response to treatments will play a major role in determining the number of treatments required. Most laser treatment plans include 6-12 treatments, with more treatment required for long-term chronic conditions. Your doctor will develop an optimal treatment plan for your condition.
BY: Web Team
Magazine
COMMENTS: No Comments
 11 Apr 2022
11 Apr 2022
What is Pediatric Ophthalmology?
Pediatric Ophthalmology
Pediatric ophthalmology is now globally recognized as a specific subspecialty. Pediatric ophthalmology care in 2018 is no longer something general ophthalmologists do as an adjunct to their predominantly adult clinical practice. It is instead delivered in dedicated pediatric ophthalmology clinics by teams of experienced childcare professionals. Advances in diagnostic and imaging techniques originally developed for adult patients (eg optical tomography (OCT), widescreen digital imaging (Optos), and modern fluorescein angiography) have expanded the options for pediatric screening.

Easily available genetic testing has changed the way we approach the screening and management of children with rare and complex eye diseases. The application of new diagnostic techniques for deep phenotyping in combination with genetic testing enhances the accuracy of diagnosis and prognosis. This now enables the introduction of true ‘customized’ medicine for children with rare eye disorders.
Equally important, a growing awareness of social and protection issues has led to improved child protection strategies across pediatric healthcare to ensure that physicians and their teams better protect children from harm.
We believe that these advances in medical and surgical care will ensure that pediatric ophthalmology remains one of the most exciting subspecialties of the future. Additionally, recent regulatory changes mean that drug companies must consider the needs of children as well as adults when seeking a license for new treatments. In the future, doctors should be able to prescribe medicines to children who have a better evidence base for efficacy and safety. We anticipate that the need to grow and enhance the currently limited evidence base for much of pediatric eye care will lead to further research and, in particular, the creation of new clinical trials in this area.
Changes in the way children are cared for in pediatric ophthalmology
Children in 2018 are rarely seen in a “general” clinic that is predominantly adults, and are more likely to be evaluated in pediatric clinics, with dedicated facilities for children, and by experienced staff with appropriate protection training. This has greatly improved the experience of caring for children and their families. The majority of consultants who deal regularly with children now have an interest in subspecialties in pediatric ophthalmology, usually after fellowship training after CCT.
Pediatric ophthalmology clinics require multidisciplinary expertise. Orthoptists have traditionally played a key role, but other allied health professionals (AHPs) such as pediatric optometrists, visionologists, and eye clinic liaison officers (ECLOs) play an important role in the delivery of high-quality pediatric ophthalmology. AHPs often work independently, both within a hospital setting and in community clinics, and support traditional outpatients by working closely with pediatric ophthalmologists. Clinics are ideally supported by pediatric nurses with appropriate training and experience. An example of current modern practice is orthopedic-led clinics/in both the community and hospital. This can include specialized follow-up clinics, for example, pediatric cataract, or uveitis led by orthoptists or optometrists, which operate in parallel with a clinic led by a consultant.
All personnel working with children now receive mandatory protection training. This helps ensure that child protection issues or signs of abuse are detected and acted upon appropriately.
Advances in Imaging and Diagnostic Tools
Accurate assessment and monitoring of eye diseases in children has always been a challenge. It can be difficult to screen young children and children with neurodevelopmental problems. They may be anxious, upset, or upset and thus fail to cooperate fully. Physical limitations can also present limitations when using tools and techniques designed for use in adults. In the past, doctors often resorted to “examination under anesthesia” (EUA) for a child in whom it was impossible to obtain an IOP measurement or when a fundus examination was similarly difficult but very important. The availability of i-Care reflex tonometry, which can be used rapidly, without eye drops, on a child with minimal cooperation [1], has significantly reduced the number of EUAs performed. This has been particularly useful for children with conditions such as glaucoma, aniridia, or facial port wine stains, where regular IOP measurement is an important part of assessment and monitoring, but repeated anesthesia carries concerns about the effect on neurodevelopment.
Advances in treatment options for children with eye diseases
The last quarter of a century has seen many changes in the way we treat eye disorders in children, both medically and surgically. There have been simultaneous changes in care pathways and massive improvements in surgical equipment and techniques.
Advances in our understanding of the natural history of strabismus and the role of refractive error in the etiology of strabismus has led to more conservative management and less strabismus surgery being performed on the children in the UK. Thus there was less need for re-operations. Alternative treatment options such as “chemical blocking” of the extraocular muscles with botulinum toxin (Botox) have been introduced over the past 30 years for the management of strabismus in children with results similar to surgery for the management of esotropia in children [4]. Botox is particularly useful in the treatment of severe medial strabismus (with or without sixth nerve palsy). This may also have contributed to less surgery and better results.
Advances in surgical instruments and techniques used in the pediatric intraocular surgery have reduced complications and improved surgical outcomes. In pediatric cataract surgery, performing posterior capsulotomy and anterior vitrectomy at the time of lensectomy reduced the rates of optic axis re-opacification. The use of smaller incisions (23 and 25 gauge), a non-traumatic surgical technique and strict anti-inflammatory regimens in the perioperative and postoperative period have reduced postoperative inflammation. It is possible, as in adults, that the use of intraocular antibiotics in surgery reduced the rate of postoperative endophthalmitis. Other major advances include a better understanding of the indications in the management of pediatric and childhood glaucoma for different surgical procedures – notably the increasing role of newer Seton devices (eg Baerveldt and Ahmed tubes) for congenital and unstable glaucoma.
BY: Web Team
Magazine
COMMENTS: No Comments
 11 Apr 2022
11 Apr 2022
Kinds of Eye Medical Procedures for Refractive Mistakes
Medical procedure is a typical therapy for vision issues. Methodology can assist with adjusting refractive mistakes. The objective of refractive eye a medical procedure is to decrease or even take out your requirement for glasses or contact focal points.

What are refractive mistakes?
Great vision relies upon how well the cornea and focal point shine light beams on the retina. Light beams should be twisted (refracted) to zero in on the retina. The retina is the light-delicate nerve layer that lines the rear of the eye. It makes beats of light beams that are sent through the optic nerve to the cerebrum.
Refractive mistakes are vision issues caused for the most part by a cornea that isn’t molded flawlessly or an eye that is longer or more limited than typical. The cornea is the unmistakable part at the front of the eye. It twists and shines light waves. Refractive blunders make light from an item not center around the retina. This causes an obscured picture. Refractive blunders can happen in sound eyes.
There are 4 sorts of refractive blunders:
1. Nearsightedness
Close by objects show up sharp. However, far off objects are not satisfactory. The eye is longer than expected from front to back. Or then again the cornea is excessively bended.
2. Farsightedness (hyperopia)
You can see far off objects plainly. Be that as it may, things very close are not satisfactory. The eye is more limited than expected. Or on the other hand the cornea is exceptionally level. The pictures center behind the retina.
3. Astigmatism
Objects are obscured from any distance. The cornea, focal point, or both are molded so that pictures don’t zero in strongly on the retina.
4. Presbyopia
This is otherwise called eye maturing. The eyes lose their capacity to change center because of the normal maturing process. This most frequently happens between the ages of 40 and 50. What’s more refractive medical procedure can’t right this issue. Medical procedure can make far off vision more clear.
Sorts of a medical procedure
Sorts of a medical procedure to address refractive blunders include:
- LASIK (laser keratomileusis)
- Photorefractive keratectomy (PRK)
- Spiral keratomileusis (RK)
- astigmatic keratoplasty (AK)
- Robotized lamellar keratoplasty (ALK)
- Laser Thermal Keratoplasty (LTK)
- Conductive keratoplasty (CK)
- Intracorneal ring (Intacs)
You can peruse more with regards to every a medical procedure beneath.
LASIK
This is a medical procedure to address partial blindness, farsightedness or astigmatism. The system reshapes the cornea utilizing an excimer laser. LASIK has supplanted numerous techniques for refractive eye a medical procedure.
This medical procedure is finished utilizing a cold excimer laser that is constrained by a PC. It likewise utilizes a little edge called a microkeratome or femtosecond laser. Utilizing one of these apparatuses, the specialist cuts a fold in the focal point of the cornea. A slim layer of tissue is taken out utilizing an excimer laser. This straightens the cornea. The fold is supplanted without join. It is reattached to the cornea in no time.
Temple directed LASIK is a high level technique for estimating visual irregularities in the eye. This procedure can be utilized to assess the eye before a medical procedure. It estimates how much light mutilates as it goes through the eye and is reflected back. This makes a visual guide of the eye and shows trouble spots. The wave front innovation permits the LASIK specialist to change the settings of the laser shaft for a more exact technique. This can give more clear vision and lessen night vision issues.
As a rule, recuperation from LASIK medical procedure is speedy, with insignificant uneasiness. Less than overwhelming pain killers and eye drops can assist with normal post-medical procedure impacts, for example,
- Dry eyes during recuperation
- Eye uneasiness in the initial 24 hours after medical procedure
- Potential complexities include:
- Revised or not entirely adjusted vision
- Sporadic astigmatism
- Corneal murkiness or glare
- photosensitivity
Powerlessness to wear contact focal points
Loss of the corneal fold and the requirement for a corneal join
- scarring
- disease
- Foggy vision or loss of vision
Photorefractive keratectomy (PRK)
This medical procedure is finished with a similar kind of excimer laser utilized in LASIK. PRK is performed to reshape the cornea to address gentle to direct partial blindness (nearsightedness).
The excimer laser bar reshapes the cornea by eliminating minuscule measures of tissue from the external surface. The technique utilizes a PC to plan the outer layer of the eye. It additionally ascertains how much tissue to be taken out. This medical procedure for the most part requires a couple of moments. It requires half a month to recuperate because of the evacuation of the corneal surface.
The most widely recognized secondary effects include:
- Eye torment that might keep going for quite some time
- A slight murkiness on the cornea following a medical procedure
- Glare or radiances around lights for a really long time after a medical procedure
Spiral keratomileusis (RK)
This technique is utilized to address gentle astigmatism. Little (cuts) are made in the cornea utilizing a jewel surgical blade. The cuts level the focal point of the cornea and change its bend. This decreases refraction. It requires half a month to mend in light of the fact that the cornea is cut off. This medical procedure was extremely normal. Be that as it may, it has nearly been supplanted by LASIK.
Potential entanglements include:
Change of vision during the initial not many months
- contamination
- Inconvenience
- A feeble cornea can crack
- Issue fitting contact focal points
- Shine around lights
- Blurring of the focal point (waterfall)
- loss of sight
Astigmatic keratoplasty (AK)
Aseptic keratotomy (AK) is basically the same as a spiral keratotomy (RK). This medical procedure is utilized to the address astigmatism. Rather than making half entry points, the eye specialist makes cuts in the cornea in a bended example.
BY: Web Team
Magazine
COMMENTS: No Comments
 09 Apr 2022
09 Apr 2022
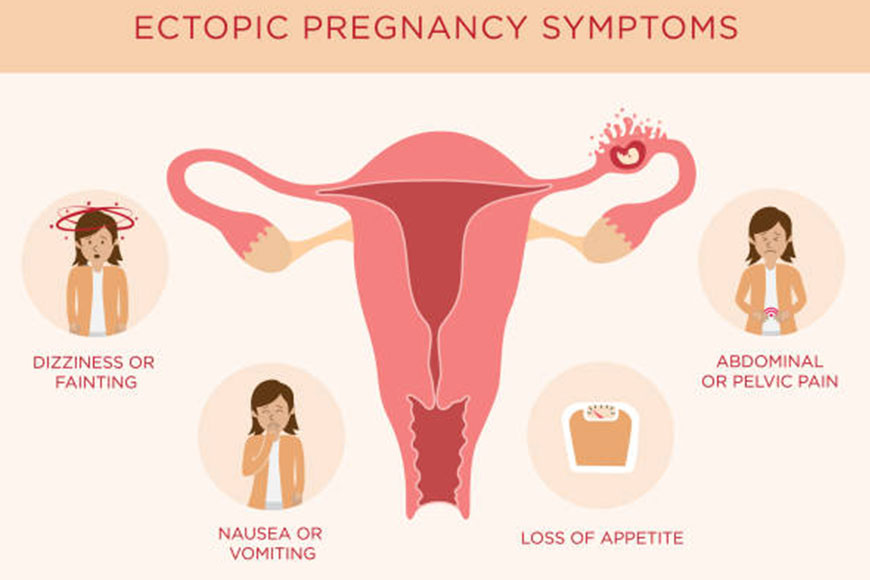
Medical and surgical management of ectopic pregnancy
After an ectopic pregnancy
Your senior obstetrician will advise you on the most appropriate treatment for you.
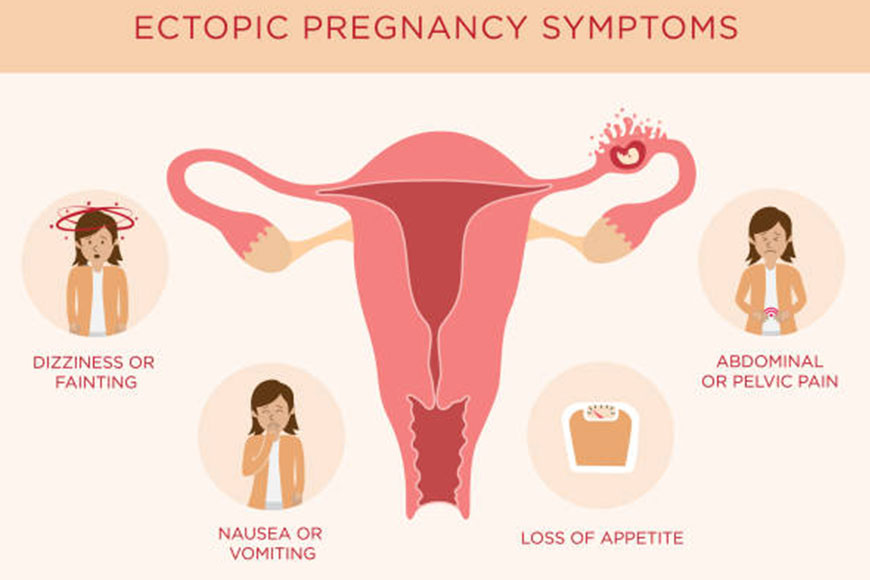
Which treatment is the best?
- How many weeks pregnant are you
- Your symptoms, and what the doctor discovers during the examination
- Ultrasound and blood test results
- Your personal opinions and preferences
- Options available at your hospital
Treatment options may include:
- Anticipatory measure (“wait and see” approach)
- The medical treatment
- surgical treatment
- Anticipatory management (“wait and see” approach)
This means waiting and seeing if the ectopic pregnancy will end on by its own. You will be carefully monitored with the frequent blood tests. This option is only suitable if the ectopic pregnancy is in a very early stage.
Call your doctor promptly if you develop any symptoms. You will usually be given a direct contact number for the emergency department or the gynecology department of the maternity hospital if you develop any symptoms.
If expectant management does not work, your doctor will suggest the medical or the surgical treatment options.
The medical treatment
Medical treatment is an injection of a drug called methotrexate. This prevents an ectopic pregnancy from developing. You don’t have to have the fallopian tube removed or part of the tube removed, and you don’t need general anesthesia.
You may need to return to the clinic or ward after a few days. You will be told who to contact if you experience any symptoms.
The main advantage of methotrexate treatment is that you do not have to undergo surgery. It may be your safest option if your BMI is very high or if you had previous surgery on your tummy (tummy).
The disadvantages include that you need to be followed up by your obstetrician for a longer period of time, perhaps three weeks. Also, 15% of the women will need a second injection of the methotrexate. Seven out of every 100 women (7%) will need surgery.
Surgical treatment
This means an operation under general anesthesia to remove the ectopic pregnancy. This is usually a laparoscopy, which is a type of keyhole surgery. A small incision is made in your abdomen and the fertilized egg is removed. The fallopian tube or part of the fallopian tube is usually removed as well.
The Open surgery (known as a laparotomy) may be needed if there is internal bleeding or in an emergency situation. This is done through a larger incision in your abdomen.
The medical team will send any tissue removed during the procedure to a laboratory for testing. Talk to the maternity hospital about what happens next.
The advantages of surgical treatment are that it treats an ectopic pregnancy more quickly and you may not need to follow up for an extended period of time. However, it does mean surgery. The recovery time from laparoscopic surgery is usually 4 to 6 weeks.
Discuss your treatment with your doctor
After you have been diagnosed with an ectopic pregnancy, unless it is an emergency, your doctor should discuss treatment options with you to allow you to make an informed decision.
Make sure you understand:
- All treatment options available to you
- No risks from a particular treatment
- Effects of a particular treatment on future pregnancies
- Don’t be afraid to ask for more information if there’s something you don’t understand.
Medical treatment protocols
The use of methotrexate to treat ectopic pregnancy was first cited in 1982.4 Several studies have followed this study and shown successful treatment of ectopic pregnancy using alternating doses of methotrexate and leucovorin.5-7 This protocol, known as the multiple dose protocol, was modified from the treatment of cancer placenta; The multiple dose regimen consisted of intramuscular injection of 1 mg/kg methotrexate with rescue factor leucovorin 0.1 mg/kg after 24 hours. Leucovorin is folinic acid, which is the active form of the folic acid.
It is used to protect cells from the effects of methotrexate and reduce its side effects. Continue this regimen on alternating days until the hCG level drops by 15% over two days. Up to 4 doses may be given to one patient, but not all 4 doses must be given. In a study by Stovall et al, 796 of 100 patients were successfully treated and none required more than four doses. The overall success rate for multidose therapy was reported in a meta-analysis by Barnhart et al of 92.7% (241 of 260 patients) with a 95% CI of 89–96%.
In 1991, a single dose protocol was proposed, but this protocol is a misnomer because more than one dose is often needed. Their protocol consisted of 50 mg/m2 of methotrexate given on day 0. Serial HCG values are plotted and compared between days 4 and 7 after treatment.
BY: Web Team
Magazine
COMMENTS: No Comments
 09 Apr 2022
09 Apr 2022
Can I give birth vaginally after a caesarean section?
If you’re pregnant again and your last baby arrived by caesarean section, you may be wondering if a vaginal delivery could be an option for you this time around. A vaginal delivery after a cesarean delivery (VBAC) is possible for many women, but there are factors that help you and your doctor decide if it’s right for you.

The most important thing to consider is the safety of you and your baby. VBAC is not always the safe for every woman.
If you attempt a vaginal birth and are at high risk of complications, it can cause serious problems for you and your baby – some of which can even be life-threatening. That is why it is important that you talk to your doctor about the risks.
For you and your doctor to consider natural childbirth, you and your baby must be healthy. You may be able to try VBAC if you are pregnant with twins, if your doctor says you are all healthy.
Your doctor may suggest that a VBAC is too risky for you to succeed in a natural birth. Risks also include any of the following:
- Obesity (your BMI of 30 or higher)
- Preeclampsia (high blood pressure during pregnancy)
- Age (usually over 35)
- Your previous caesarean delivery was in the last 19 months
- The fetus is very large
- Previous C-section scar
An important detail that you and your doctor should discuss is the type of C-section scar you have on your uterus. (This may be the same type of scar you have on your stomach, but it may go in a different direction.) Doctors make incisions (cuts in the abdomen and uterus) in the two different directions during a C-section:
Cutting my head goes from top to bottom
A cross cut goes from side to side
If the C-section scar is vertical, you cannot try VBAC. There is a high risk that your scar will rupture (rupture or rupture) when attempting a vaginal birth, which can cause significant harm to you and your baby. You will need to have the C-section again.
If your C-section scar is low and transverse, your doctor may allow you to try VBAC, if your other risk factors are low.
Hospital affairs
Check with your doctor early to see if the hospital you’re using allows women to try VBAC. Not every hospital does this.
Although the risk of your old scar rupturing during a VBAC is low, the hospital must be prepared to handle the emergency that may arise if this occurs. Some hospitals are simply not prepared to deal with it.
Low risk vs no risk
There is a very small chance for every woman trying a VBAC that her uterus will rupture, even if she has a low, transverse C-section scar and is otherwise healthy. Doctors cannot be 100% sure whether or not this may happen to you.
Although lacerations occur in less than 1% of VBAC attempts, some women do not want to try it at all, because if they do occur, they can be very dangerous. You need to weigh your options and talk to your doctor before deciding what to do.
VBAC Benefits
If a VBAC is an option for you and you like the idea of trying a natural birth, there are many reasons you might want to try it. There is a good chance of success: About 70% of women who try to have their children vaginally. For the rest, a cesarean delivery is required, because of the problems that appear during the attempt.
You may want to give VBAC a try for many reasons because if it is successful, it will have the following benefits:
- Does not require surgery
- Less blood loss
- faster recovery
- Decreased chance of infection
- You are less likely to get an injury to your bladder or intestines
- You are likely to have fewer problems with childbirth in the future
A case of scar rupture can be fatal for both the mother and the baby. To avoid this, Dr. Bandana stated that the following criteria should be followed:
- The gap between the two pregnancies is important when considering a vaginal delivery after a cesarean delivery. A gap of at least 18 months is required for vaginal delivery after cesarean delivery. You can’t even attempt a natural delivery if the gap is less than that.
- The weight of the baby in the ninth month will also determine whether a natural birth after a cesarean delivery is possible or not.
- The baby should be positioned face down for vaginal delivery after cesarean delivery.
- There should be a spacious passage for the child. The pelvis should be suitable for the passage of the child.
- The reason for the cesarean delivery during the first pregnancy should also be known. This helps diagnose whether the same risk factors are present during the current pregnancy.
- The sequence and thickness of the scar should also be checked for vaginal delivery after cesarean delivery.
- Deviation from any of the above risk factors can be fatal for both the mother and the baby. Obesity and women over the age of 40 are also at risk of stillbirth during vaginal delivery after a cesarean delivery.
BY: Web Team
Magazine
COMMENTS: No Comments
 09 Apr 2022
09 Apr 2022
Electrodiagnostic Studies are the Extension of the Clinical Examination
Tests do not replace a careful history and the examination of the patient
NCS/EMG is an extension of clinical assessment
These observations may seem implausible to those who do not take these tests and see electrodiagnostic tests as the “black box” from which answers magically appear. However, neurophysiology is certainly used in the same way as a clinical examination to solve clinical problems, and it complements, rather than replaces, clinical evaluation. On clinical examination, locate the lesion by evaluating the distribution of weakness, reflex changes, and sensory loss. Neurophysiologically, it examines not only the distribution but also the type of abnormalities detected in nerve conduction and EMG studies. Neurophysiology can be thought of as a clinical examination with the ability to “examine” nerves and muscles in a different way.

There are some obvious similarities with clinical examination:
Locating a clinically significant impairment is usually more straightforward than locating a milder degree of impairment as it tends to be less certain in distinguishing between mild weakness and normal strength. Likewise, ‘soft’ sensory signs tend to be more difficult to localize. These problems manifest themselves Neurophysiologically – the most significant lesion is easy to localize as the neurophysiological abnormalities are more pronounced.
If cooperation is difficult to obtain on clinical examination, it is likely even more so when doing neurophysiology – especially electromyography which requires a high level of patient cooperation.
On examining a patient, you are often able to exclude some clinical findings that are related to known prior pathology – eg, mild foot drop from previous L5 radiculopathy; A neurophysiologist should do the same, so please tell them.
Both NCS/EMG and clinical examination is operator dependent.
The NCS/EMG is particularly useful in locating the peripheral nervous system deficit found on clinical examination. So:
If you can’t frame your question in anatomical terms, which is how a neurophysiologist would try to answer it, then wonder why the test is required at all.
If you can confidently localize the lesion on clinical examination alone, will you get additional useful information from the NCS/EMG order?
Oftentimes neurophysiological studies can locate the lesion more accurately than examination alone, but they do not identify the cause. This usually requires further investigations and neurophysiological studies may add nothing to the diagnosis if these other tests are diagnostically positive. For example, neurophysiological confirmation of L5 radiculopathy may contribute little if the magnetic resonance image (MRI) of the lumbosacral spine clearly demonstrates compression of the L5 root. If you are going to have other tests, consider whether the NCS/EMG will add to the diagnosis. In the era of the ‘programmed investigation approach’ remember that ‘mass confinement’ tests and thus failure to value the investigative pathway is a poor and ineffective use of diagnostic resources.
Before looking at the role that NCS/EMG plays in different clinical situations, it is useful to think a little about the tests themselves and make some observations about how we use investigations in general.
Tests
Evidence-based medicine suggests that we must understand the special features of diagnostic tests, such as sensitivity (the ability to detect those with disease) and specificity (the ability to detect those who do not). To account for these, we ask that the test be compared to the accepted gold standard.
This leads to the first problem for NCS/EMG. For some conditions – eg, chronic inflammatory demyelinating colonic radiculopathy (CIDP) or multifocal motor neuropathy with conduction block – the NCS/EMG is an essential part of the definition of these conditions making sensitivity and specificity calculations somewhat circular, although Attempts to evaluate different combinations of diagnostic criteria 1 For other conditions, such as carpal tunnel 2 or ulnar neuropathy of the cubital tunnel, 3 While NCS/EMG is not the only way to confirm the diagnosis, it is probably the most robust non-invasive method. In other cases, another method can provide a more accurate diagnosis – eg, cervical radiculopathy where MRI or surgical findings can provide the gold standard.
Paradoxically, this means that the circumstances in which there is the best published evidence of sensitivity and specificity are those in which there is another, more specific method for achieving the diagnosis, this being used as the gold standard against which NCS/EMG can be compared. Cervical and the lumbar radiculopathy are clear examples of this.
BY: Web Team
Magazine
COMMENTS: No Comments