 09 Apr 2022
09 Apr 2022
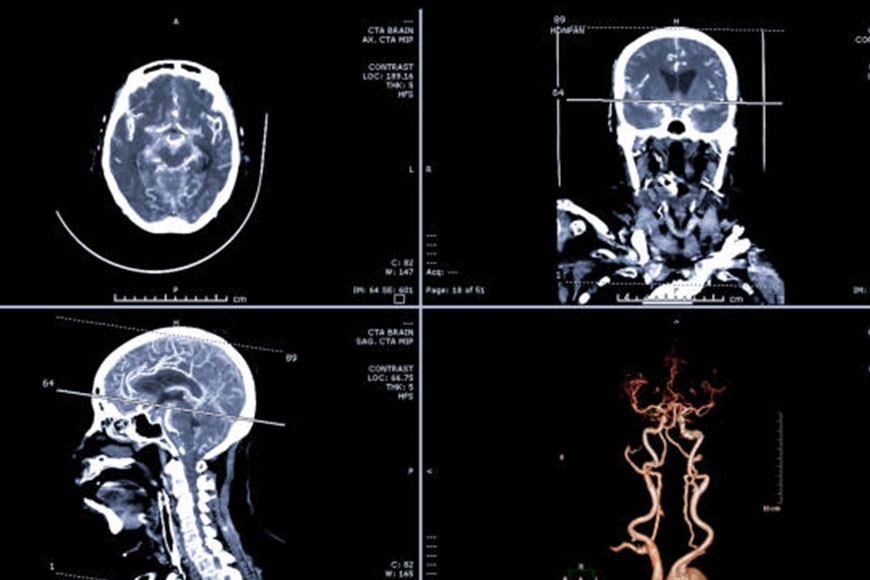
What is cerebral angiography?
Cerebral angiography is a demonstrative test that utilizes X-beams. It creates a cerebral angiogram, or a picture that can assist your PCP with tracking down blockages or different anomalies in the veins in the head and neck. Blockages or anomalies can prompt a stroke or draining in the cerebrum.
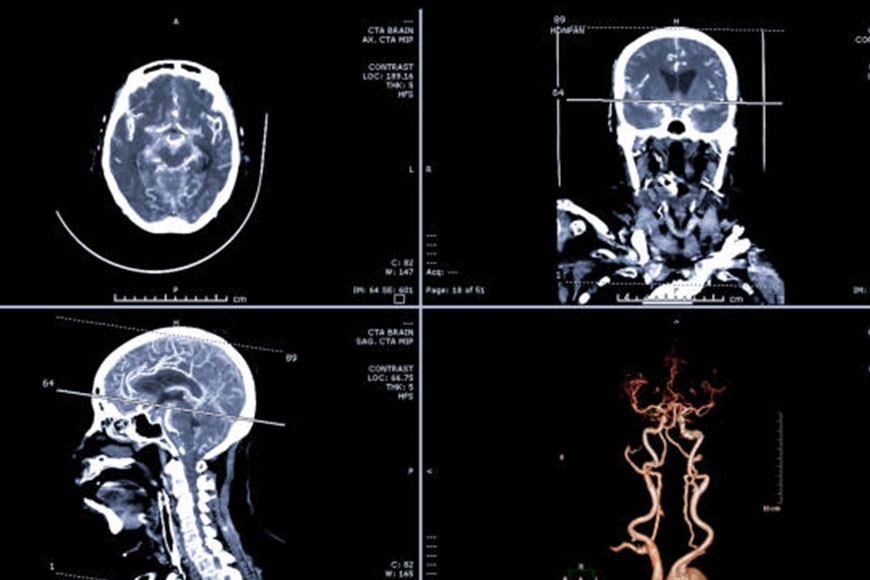
In this test, your primary care physician infuses a differentiation medium into your blood. The difference material assists the X-beams with making an unmistakable image of the veins so your PCP can recognize any blockages or anomalies.
Services
Not every person with stopped up veins needs a cerebral angiography. It’s normally possibly done in the event that your primary care physician needs more data to design your treatment after different tests. This is on the grounds that it is intrusive and conveys a few dangers.
Angiography may likewise be utilized to assist with treating a few conditions including veins in the neck and mind. Cerebral angiography can help analyze:
- aneurysm
- Arteriosclerosis
- Blood vessel venous distortions
- Vasculitis or vasculitis
- mind cancers
- blood clumps
- breaks in the coating of the course
Cerebral angiography may likewise assist your PCP with tracking down the reason for a portion of your indications, including:
- mind assault
- Extreme cerebral pain
- cognitive decline
- hazy
- Wooziness
- Obscured or twofold vision
- shortcoming or deadness
- Loss of equilibrium or coordination
Instructions to plan
Converse: with your primary care physician regarding how to plan. You will most likely be unable to eat or drink after 12 PM before the method.
Before the methodology, your PCP may likewise request that you quit taking prescriptions that can build your danger of dying. These include:
- blood thinners
- anti-inflamatory medicine
- Non-steroidal mitigating drugs
In the event that you are breastfeeding, express your milk before the technique, and don’t breastfeed your child again for no less than 24 hours. This holding up time will give the differentiation material chance to leave your body.
Alert your primary care physician
Let your primary care physician know if you have any sensitivities or ailments. Certain individuals are oversensitive to the difference material utilized during the strategy. Let your PCP know if you have any sensitivity, including aversions to sedation or difference material given for a CT filter. Your PCP might recommend hostile to sensitivity prescriptions before the test.
Certain illnesses and ailments can build the danger of inconveniences during the test. Assuming you have diabetes or kidney sickness, the difference material can make impermanent harm your kidneys. Assuming that you are pregnant or figure you may be, you ought to get some information about radiation openness during the test.
What’s in store during the activity?
Your medical services group for this test might incorporate a radiologist, neurosurgeon or nervous system specialist who spends significant time in interventional radiology and a radiology expert.
A great many people are quieted before the system. Others – particularly youngsters – are given general sedation. This is on the grounds that you must be still for the test to be powerful. The calming will assist you with feeling loose, and you might nod off.
During the method, your head will be immobilized with tape, tape, or blocks. It is vital to stay as yet during the test.
To begin, your primary care physician will disinfect a region of your crotch. They’ll embed a catheter (a long, adaptable cylinder) and string it through a vein into the carotid corridor. This is the vein in your neck that conveys blood to your cerebrum.
The difference color will course through the catheter into the supply route. From that point, it will make a trip to the veins in your mind. You might feel warm as the difference color courses through your body. Then, at that point, the specialist takes a few x-beams of the head and neck. While the sweeps are being performed, you might be approached to stay still or even pause your breathing for a couple of moments.
Then, your primary care physician will eliminate the catheter and spot a swathe over the addition site. The whole interaction for the most part requires one to three hours.
Hazards
Cerebral angiography conveys a few intriguing however genuine dangers. They include:
- Stroke (assuming the catheter slackens the plaque inside a vein)
- Vascular harm, including vein hole
- Blood clusters can conform to the tip of the catheter
- Make certain to examine all hazards cautiously with your PCP.
Follow-up after cerebral angiography
After the system, you’ll go to the recuperation room, where you’ll lie still for two to six hours prior to returning home. At home, be mindful so as not to lift weighty items or exhaust yourself for somewhere around seven days.
Call your primary care physician immediately assuming you experience any of the accompanying:
- Indications of a stroke, including slurred discourse, shortcoming, deadness, or vision issues
- Redness and expanding at the catheter inclusion site
- Expanding or frigidity in the leg or foot
- Source
Discombobulating
At the point when your outcomes are free, the radiologist will decipher them. Your primary care physician will impart these outcomes to you and talk about follow-up tests or treatment.
BY: Web Team
Magazine
COMMENTS: No Comments
 09 Apr 2022
09 Apr 2022
What are Glomerular diseases?
Glomerular disease is caused by conditions that affect a specific part of the kidneys called the glomeruli. The glomeruli are a small network of blood vessels that are the “cleaning units” of your kidneys. They filter waste and remove excess fluid from the blood. When the glomeruli are damaged and cannot function as they should, it is called glomerulosclerosis.

Many diseases and conditions can damage the glomeruli. There are two broad terms used to describe many forms of damage to the glomeruli:
- Glomerulonephritis, inflammation (swelling) of the glomeruli.
- Glomerulosclerosis, scarring/hardening of the glomeruli.
- Glomerulosclerosis can damage the kidneys and, in some cases, lead to kidney failure.
How do the glomeruli work in your kidney?
The kidneys, two bean-shaped organs to the left and right of the spine below the rib cage, are your body’s main filters.
The blood enters the kidneys through the arteries. Once in the kidneys, the arteries branch off and the blood passes into the network of small annular blood vessels called glomeruli. Each glomerulus is connected to the opening of a small fluid-collecting tube called a microtubule. Each glomerulus unit is called a nephron. There are about one million nephrons in each of the kidney.
Properly functioning glomeruli work by keeping blood cells and protein circulating in the bloodstream, where your body needs them. Meanwhile, the glomeruli filter waste and excess water, to pass fluid into the tube (which turns into urine). Urine leaves the kidneys through larger tubes called ureters, which carry urine to the bladder.
How does glomerulosclerosis interfere with kidney function?
Glomerular disease damages the glomeruli, affecting their ability to function properly. Instead of retaining protein and red blood cells in the blood, the damaged glomeruli cause some of these products to leak into the urine. One of the functions of blood proteins, such as albumin, is to transport excess fluid from the body into the bloodstream so that it can be filtered by the kidneys and removed from the body as urine. Not having enough protein in your bloodstream keeps excess fluid in your body, causing swelling in areas such as the face, hands, feet, abdomen, and ankles.
The damaged glomeruli also cannot filter waste products and these products begin to build up in the blood.
What causes glomerulosclerosis?
Causes of glomerulosclerosis include:
- An infection, medication, or chemical that is harmful to your kidneys.
- Diseases affecting the whole body, including the kidneys.
- Diseases that cause the swelling or scarring of the nephron or the glomerulus.
- Unknown cause.
What are the signs and symptoms of glomerulosclerosis?
Signs of glomerulosclerosis include one or more of the following:
- The Foamy urine (a sign of the protein in the urine [proteinuria]).
- Pink or light brown urine (a sign of blood in the urine [hematuria]).
- Swelling in your face/around the eyes (especially in the morning), hands, feet, or ankles (especially at the end of the day). This swelling is called edema.
How is glomerulosclerosis diagnosed?
After a thorough physical and medical history, your health care provider will order several tests, including:
- A urine test (urinalysis), to check for a high protein level, presence of red blood cells, and level of white blood cells (may indicate infection or inflammation).
- Blood tests, to check for low levels of protein, creatinine (kidney function) and levels of urea nitrogen (a waste product). A calculation, called the glomerular filtration rate (GFR), is done to determine if your kidneys are filtering properly.
If these lab tests indicate kidney damage, your health care provider may order:
- Additional blood tests for possible causes such as infections or autoimmune diseases.
- Imaging tests, including ultrasound, to see if the shape or the size of the kidneys is abnormal.
- Kidney biopsy, which involves using a needle to remove small pieces of tissue for viewing under a microscope.
What diseases and conditions cause glomerulosclerosis and how are they treated?
Many diseases can lead to glomerulosclerosis. The goal of treatment is to treat the underlying cause (if it can be identified) to protect your kidneys from further damage. Here are some general categories of diseases that can cause glomerulosclerosis and examples and treatments for each.
Autoimmune diseases
These are diseases in which the body’s immune system attacks itself. These diseases can affect your entire body or may attack only certain organs or areas of your body. Autoimmune diseases that affect the kidneys which include:
1. Systemic lupus erythematosus (SLE) (also known as lupus)
This autoimmune disease affects many parts of the body. In the kidneys, it causes lupus nephritis, an inflammation of the glomeruli. The inflammation causes scars that prevent the kidneys from working properly. Anti-inflammatory treatment includes immunosuppressive drugs such as mycophenolate mofetil or cyclophosphamide with the corticosteroid prednisolone.
2. Goodpasture’s Syndrome
An autoimmune disease: that attacks the kidneys and lungs. In the kidneys, it causes glomerulonephritis, which is an inflammation of the glomeruli and can lead to permanent kidney damage. Treatments include immunosuppressive medications and plasmapheresis (a process to remove the antibodies that attack your body).
3. IgA nephropathy
With this autoimmune disease, a specific part of the immune system called immunoglobulin A (IgA) antibodies forms deposits in the glomeruli. These deposits cause inflammation. Treatments include ACE inhibitors or angiotensin receptor blockers.
4. Hereditary nephritis
Alport syndrome: It is an inherited condition that causes chronic glomerular disease along with impaired hearing or vision. It affects both men and women. Men suffer more from chronic kidney disease, which can be diagnosed in their twenties; Total kidney failure most often occurs around the age of 40. Treatments include medications to control the blood pressure.
BY: Web Team
Magazine
COMMENTS: No Comments
 09 Apr 2022
09 Apr 2022
Acute kidney disease treatment
Diagnose
If your signs and symptoms suggest that you have the acute kidney failure, your doctor may recommend certain tests and procedures to verify your diagnosis. These may include:
1. Urine output measurements
Measuring the amount of urination within 24 hours may help your doctor determine the cause of kidney failure.
2. Urine tests
Analyzing a sample of your urine (urinalysis) may reveal the abnormalities that suggest kidney failure.
3. Blood tests
A sample of your blood may reveal a rapid rise in levels of urea and creatinine — two substances used to measure kidney function.
4. Imaging tests
Imaging tests such as ultrasound and CT may be used to help your doctor see your kidneys.

Take a sample of kidney tissue for examination. In some cases, your doctor may recommend a kidney biopsy to remove a small sample of kidney tissue for examination in a laboratory. Your doctor inserts a needle through your skin and into your kidney to remove sample.
Treatment
Treatment for acute kidney failure usually requires a hospital stay. Most people with the acute kidney failure are already hospitalized. How long you’ll be in the hospital depends on the cause of your acute kidney failure and how quickly your kidneys recover.
In some cases, you may be able to recover at the home.
Treating the underlying cause of a kidney injury
Treatment for acute kidney failure involves identifying the disease or injury that originally damaged your kidneys. Treatment options depend on cause of the kidney failure.
Treat complications until the kidneys recover
Your doctor will also work to prevent complications and allow your kidneys to heal. Treatments that help prevent complications include:
1. Treatments to balance the amount of fluid in the blood
If the cause of your acute kidney failure is a lack of fluid in the blood, your doctor may recommend intravenous (IV) fluids. In other cases, acute kidney failure may cause too much fluid, resulting in swollen arms and legs. In these cases, your doctor may recommend medications (diuretics) to make your body expel the extra fluid.
2. Medicines to control potassium in the blood
If your kidneys aren’t filtering potassium from the blood properly, your doctor may prescribe calcium, glucose, or sodium polystyrene sulfonate (Kunix) to prevent high levels of potassium from building up in the blood. Too much potassium in the blood can lead to an irregular heartbeat (arrhythmia) and muscle weakness.
3. Medicines to restore calcium levels in the blood
If the levels of calcium in your blood are too low, your doctor may recommend a dose of calcium.
4. Dialysis to remove toxins from the blood
If toxins build up in your blood, you may need temporary dialysis — often referred to as hemodialysis — to help remove toxins and extra fluid from your body while your kidneys recover. Hemodialysis may also help remove excess potassium from your body. During hemodialysis, a machine pumps blood out of the body through an artificial kidney (dialysis machine) to filter waste. Then the blood returns to your body.
Depending on your condition, your dietitian may recommend the following:
1. Choose foods that are low in potassium
A dietitian may recommend choosing foods that are low in potassium. Foods rich in the potassium include bananas, oranges, potatoes, spinach, and tomatoes. Examples of foods low in potassium include apples, broccoli, peppers, grapes, and strawberries.
2. Avoid products with added salt
Reduce the amount of sodium you eat each day by avoiding products with added salt, including many prepared foods, such as frozen dinners, canned soup, and fast foods. Other foods with added salt include salty snack foods, canned vegetables, processed meats, and cheese.
3. Reducing phosphorous
Phosphorous is a mineral found in foods, such as whole-grain bread, oatmeal, bran cereal, dark cola, nuts, and peanut butter. Having too much phosphorous in your blood can weaken your bones and cause your skin to itch. A dietitian can give you specific recommendations on phosphorous and how to limit it in your particular case.
As your kidneys recover, you may no longer need to go on a special diet, although healthy eating remains important.
Preparing for your appointment
Most people are already hospitalized when they develop the acute kidney failure. If you or a loved one develops signs and symptoms of kidney failure, discuss your concerns with your doctor or nurse.
If you’re not in the hospital, but have signs or symptoms of kidney failure, make an appointment with your family doctor or a general practitioner. If your doctor suspects you have kidney problems, you may be referred to a doctor who specializes in kidney diseases (nephrologist).
BY: Web Team
Magazine
COMMENTS: No Comments
 09 Apr 2022
09 Apr 2022
Long-term care safety guideline
The patient wellbeing field has essentially centered on further developing security in emergency clinic and mobile settings. However an enormous and developing number of Americans who don’t need emergency clinic level consideration yet can’t be securely focused on at home dwell in settings alluded to as long haul care. These settings incorporate gifted nursing offices (SNFs), ongoing restoration offices, and long haul intense consideration medical clinics. There were more than 1.6 million inhabitants of SNFs in 2011, and long haul intense consideration clinics affirmations among Medicare recipients have dramatically increased throughout recent years.

Patients in long haul care settings might be especially helpless against wellbeing issues over their consideration. Patients requiring care in long haul care offices are excessively more established and persistently sick and they frequently enter long haul care after an intense hospitalization. Medical care usage in the wake of entering long haul care is high-a review by the Office of the Inspector General (OIG) saw that as almost 25% of Medicare SNF occupants require hospitalization every year.
Each sort of long haul care setting offers various types of assistance and is reasonable for various kinds of patients:
Long haul intense consideration clinics care for medicinally complex patients expected to require care for weeks to months. These patients are regularly constantly fundamentally sick, generally normally recuperating from a hospitalization that incorporated an emergency unit. These offices offer types of assistance basically the same as intense consideration medical clinics, including the capacity to really focus on patients requiring mechanical ventilation, complex injury care, or hemodialysis. The offices might be unattached or appended to an intense clinic, and they are dependent upon the equivalent authorizing and credentialing necessities as conventional medical clinics. Patients at long haul intense consideration clinics by and large require day by day assessment by a doctor.
Long term restoration offices care for patients recuperating from a medical procedure, injury, or an intense sickness. They give escalated restoration patients should have the option to endure 3 hours of physical or word related treatment every day fully intent on reestablishing patients to their premorbid utilitarian status. Care is managed by a multidisciplinary group that incorporates a doctor, ordinarily an expert in restoration medication.
Gifted nursing offices for the most part care for patients who might be constantly sick however are viewed as restoratively steady. By and large, these patients don’t need every day assessment by a doctor however require administrations like non-intrusive treatment or wound consideration.
Patients frequently enter long haul care after an intense hospitalization. Information from 2011 shows that almost 40% of Medicare recipients are released to some type of long haul care office most frequently a SNF-after emergency clinic release. In this manner, the term post-acute care is additionally used to allude to the usage of long haul care offices to give proceeding with care after hospitalization. Postacute patients address an expanding extent of the in general SNF patient populace, and these patients-who are regularly medicinally intricate and fragile, may burden the capacity of SNFs to give safe consideration. Because of this multitude of elements, the security field is beginning to inspect and address wellbeing issues looked by patients in long haul care.
Wellbeing Concerns in Long-term Care
Preventable antagonistic occasions are normal in long haul care. A 2014 report by the OIG saw that as 22% of Medicare recipients in SNFs encountered an antagonistic occasion during their visit, a big part of which were preventable. The greater part of the patients who encountered an antagonistic occasion at a SNF required hospitalization. A different OIG report tracked down a much higher occurrence of antagonistic occasions at recovery offices. Among these are perils that are very much recorded in more established patients, for example, drug blunders, medical care related diseases, wooziness, falls, and tension ulcers. Unfavorable medication occasions were the most well-known sort of antagonistic occasion in the OIG concentrate as well as in different investigations of long haul care populaces. While patient intricacy clarifies a portion of these occasions, it is likewise important that electronic supplier request section and other drug security systems have not been executed as generally in SNFs as in emergency clinics. Medical care related diseases especially catheter-related urinary parcel contaminations are additionally normal in long haul care, and endeavors are in progress to resolve this issue. A WebM&M critique examines the sorts of unfavorable occasions that happen in SNF patients in more detail and gives proof based proposals for forestalling these damages.
Laying out a hearty culture of wellbeing is fundamental for limiting patient damage. Tragically, wellbeing society in some drawn out care offices is more unfortunate than that found in clinics and wandering facilities. A recent report utilizing the AHRQ Hospital Survey on Patient Safety Culture observed that nursing home heads apparent security culture in their offices to be lower than clinic benchmarks across essentially all spaces of the study. AHRQ in this manner fostered a security culture overview instrument for nursing homes and has delivered semiannual benchmarking information starting around 2008. The latest (2014) information shows generally improvement in long haul care security culture, however respondents actually raise worries about expected patient mischief due to deficient staffing and an excessively correctional culture.
BY: Web Team
Magazine
COMMENTS: No Comments
 09 Apr 2022
09 Apr 2022
What is long term care?
Long term care includes the variety of the services designed to meet the person’s health or the personal care needs over a short or long period of time. These services help people to live as the independently and safely as possible when they can no longer perform daily activities on their own.

Long-term care is provided in different settings by different providers, depending on the person’s needs. Most long-term care at home is provided by unpaid family members and friends. It may also be given in a facility such as a nursing home or in the community, for example, at an adult day care center.
The most common type of long-term care is personal care – assistance with daily activities, also called “activities of daily living.” These activities include bathing, dressing, grooming, toileting, eating, and moving – e.g. getting out of bed and sitting in a chair.
Long term care also includes the community services such as meals, adult day care, and transportation services. These services can be provided free of the charge or for a fee.
People often need long-term care when they have a serious and persistent health condition or disability. The need for long-term care can arise suddenly, such as a heart attack or stroke. However, it most often develops gradually, as people get older and weaker or as disease or disability worsens.
Who needs long-term care?
It is difficult to predict how much or what type of long-term care a person may need. Several things increase the risk of the needing long term care.
- The risks generally increase as people get older.
- Women are at greater risk than men, mainly because they often live longer.
- Social status. Singles are more likely to need sponsorship from a paid provider than married people.
- Poor diet and exercise habits can increase a person’s risk of infection.
- Health and family history. These factors also affect the risk.
What are the different types of home long-term care services?
Long-term care at home includes health, personal and support services to help people stay home and live as independently as possible. Most long-term care is provided either in the home of the person receiving services or at the home of a family member. Home services may be short-term – for someone recovering from surgery, for example – or long-term for people who need ongoing help.
Most home services include the personal care, such as help with bathing, dressing, taking medications, and supervision to make sure the person is safe. Family members, partners, friends and the neighbors provide most of this type of care.
Long-term care services may also be provided at home by paid care providers, including informally located caregivers, and health care professionals such as nurses, home health care aides, therapists, and housewives, who are hired through home health care agencies. These services include: home health care, housewife services, friendly visitor/escort services, and emergency response systems.
Home health care
Home health care includes part-time medical services that a physician orders for a specific condition. These services may include nursing care to help a person recover from surgery, accident, or illness. Home health care may also include physical, occupational or speech therapy and temporary home health assistance services. These services are provided by home health care agencies approved by Medicare, a government insurance program for people over 65.
Housewife and personal care services
Home health agencies offer housewife and personal care services that can be purchased without a doctor’s order. Housewife services include helping with meal preparation and household chores. Personal care includes the assistance with bathing and the dressing. Agencies do not have to obtain Medicare approval to provide these types of services.
Friendly visitor and top service attendant
Friendly visitor/escort services are usually provided by volunteers who regularly make short visits (less than 2 hours) to someone who is vulnerable or living alone. You can also purchase these services from the home health agencies.
Senior Transportation Services
Transportation services help people get to and from the medical appointments, shopping centers, and other places in the community. Some senior apartment complexes and community groups offer transportation services. Many public transportation agencies have services for people with disabilities. Some services are free. Others charge a fee.
Emergency medical alert systems
Emergency response systems automatically respond to medical and other emergencies via electronic screens. The user wears a necklace or bracelet with a push-button in case of emergency. Pressing the button calls emergency help home. This type of service is especially useful for the people who live alone or are at the risk of falling. A monthly fee is charged.
Planning for long-term care
You cannot know for sure if you will need long-term care. You may never need it, but the unexpected accident, illness or injury can change your needs, sometimes suddenly. The best time to think about the long term care is before you need it.
Planning for access to long-term care gives you time to learn about services in your community and their costs. It also allows you to make important decisions while still being able to.
People with Alzheimer’s disease or other cognitive impairments should start planning for long-term care as soon as possible.
BY: Web Team
Magazine
COMMENTS: No Comments
 01 Apr 2022
01 Apr 2022
What is Asthma and its Treatment
Physical exam
Your doctor will do a physical exam to rule out other possible conditions, such as a respiratory infection or chronic obstructive pulmonary disease (COPD). Your doctor will also ask you questions about the signs and symptoms and about any other health problems.

Lung function tests
You may have lung function tests to determine how much air is going in and out as you breathe. These tests may include:
Spirometry
This test estimates narrowing of the bronchial tubes by checking how much the air you can exhale after a deep breath and how fast you can exhale.
Flow peak
A peak flow meter is a simple device that measures how hard it is to exhale. Lower than normal peak flow readings are a sign that your lungs may not be working well and that your asthma may be getting worse. Your doctor will give you instructions on how to track and manage low peak flow readings.
Lung function tests are often done before and after you take a medicine to open your airway called a bronchodilator (brong-koh-DIE-lay-tur), such as albuterol. If your lung function has improved with a bronchodilator, you likely have asthma.
Additional tests
Other tests to diagnose asthma include:
1. The methacholine challenge
Methacholine is a known asthma trigger. When inhaled, this will narrow the airway slightly. If you react to methacholine, you likely have asthma. This test may be used even if the initial lung function test is normal.
2. Imaging tests
A chest X-ray can help identify any structural abnormalities or diseases (such as infections) that can cause or worsen breathing problems.
3. Allergy test
Allergy tests can be done with a skin exam or a blood test. They tell you if you are allergic to pets, dust, mold, or pollen. If an allergen is identified, your doctor may recommend allergy shots.
4. Nitric oxide test
This test measures the amount of the nitric oxide gas in your breath. When your airways are inflamed — a sign of asthma — you may have higher than normal levels of nitric oxide. This test is not widely available.
5. Sputum eosinophils
This test looks for certain white blood cells (eosinophils) in the mixture of saliva and mucus (sputum) you produce when you cough. Eosinophils appear when symptoms develop and become visible when stained with pink pigment.
Provocative tests for exercise and cold-induced asthma
In these tests, your doctor measures airway obstruction before and after you perform vigorous physical activity or take several breaths of cold air.
How is asthma classified?
To classify the severity of your asthma, your doctor will look at how often you have signs and symptoms and how severe they are. Your doctor will also consider the results of a physical exam and diagnostic tests.
Determining the severity of your asthma helps your doctor choose the best treatment. Asthma severity often changes over time, requiring adjustments in treatment.
Treatment
Prevention and long term control are key to stopping asthma attacks before they start. Treatment usually involves learning to recognize triggers, taking steps to avoid triggers and tracking your breathing to make sure the medications you’re taking keep your symptoms under control. If your asthma flares up, you may need to use an inhaler for quick relief.
1. Pharmaceutical
Which medications are right for you depends on a number of things — your age, your symptoms, your asthma triggers, and what’s best for controlling your asthma.
Long-term preventive medications reduce the swelling (inflammation) in the airway that leads to symptoms. Quick-relief inhalers (bronchodilators) quickly open swollen airways that limit breathing. In some cases, the allergy medications are necessary.
Long term asthma control medications, generally taken daily, are the cornerstone of asthma treatment. These medications keep your asthma under control on a daily basis and reduce your chance of having an asthma attack. Types of long-term disease control medications include:
2. Inhaled corticosteroids
These medications include fluticasone propionate (Flovent HFA, Flovent Diskus, Xhance), budesonide (Pulmicort Flexhaler, Pulmicort Respules, Rhinocort), ciclesonide (Alvesco), beclomethasone (Qvar Redihaler), mometasone (Asmanex flutic TwisHFA, Asmanexhaler Twis) Ellipt.
You may need to use these medications for several days to weeks before you get maximum benefit. Unlike oral corticosteroids, the inhaled corticosteroids have a relatively low risk of serious side effects.
3. Leukotriene rates
These oral medications including montelukast (Singulair), zafirlukast (Accolate) and zileuton (Zyflu) — help relieve asthma symptoms.
Montelukast has been linked to psychiatric reactions, such as agitation, aggression, hallucinations, depression, and suicidal ideation. Seek medical advice immediately if you experience any of these reactions.
4. Combined inhalers
These medications — such as fluticasone-salmeterol (Advair HFA, Erdo Digihaler, others), budesonide-formoterol (Symbicort), formoterol-mometasone (Dulera) and fluticasone furoate-vilanterol (Brio Ellipta) — contain a long-acting beta-agonist corticosteroid.
5. Theophylline
Theophylline (Theo-24, Elixophyllin, and Theochron) is a daily pill that helps keep the airways open by relaxing the muscles around airways. It is not used as often as other asthma medications and requires regular blood tests.
Quick relief medications are used as needed for rapid, short term relief of symptoms during an asthma attack. They can also be used before exercise if recommended by your doctor. Types of quick-relief medications include:
1. Short-acting beta-agonists
These relaxing inhaled bronchodilators work within minutes to quickly relieve symptoms during an asthma attack. They include albuterol (ProAir HFA, Ventolin HFA, and others) and levalbuterol (Xopenex, Xopenex HFA).
Short-acting beta-agonists can be taken using a hand-held inhaler or nebulizer, a machine that turns asthma medications into a fine mist. It is inhaled through a face mask or mouthpiece.
2. Anticholinergic agents
Like other bronchodilators, ipratropium (Atrovent HFA) and tiotropium (Spiriva, Spiriva Respimat) work quickly to relax the airways immediately, making breathing easier. Mostly used for emphysema and chronic bronchitis, but can be used to treat asthma.
3. Oral and intravenous corticosteroids
These medications — which include prednisone (Prednisone Intensol, Rayos) and methylprednisolone (Medrol, Depo-Medrol, Solomedol) — relieve airway inflammation caused by severe asthma. They can cause serious side effects when used long-term, so these medications are only used short-term to treat severe asthma symptoms.
BY: Web Team
Magazine
COMMENTS: No Comments
 01 Apr 2022
01 Apr 2022
Acute respiratory infection
What is acute respiratory infection?
An acute respiratory infection is an infection that may interfere with the normal breathing. It can affect only the upper respiratory tract, which begins in the sinuses and ends at the vocal cords, or only the lower respiratory tract, which begins at the vocal cords and ends at your lungs.

This infection is especially dangerous for children, the elderly, and people with compromised immune systems.
What are the symptoms of acute respiratory infection?
The symptoms you experience will be different if it is an infection in the lower or upper respiratory tract. Symptoms can include:
- Congestion, either in the sinuses or the lungs
- Runny nose
- cough
- sore throat
- body aches
- fatigue
Call your doctor if you experience:
- Fever over 39°C and chills
- breathing difficulties
- Dizziness
- Unconsciousness
What causes acute respiratory infection?
There are several different causes of the acute respiratory infection.
Causes of an upper respiratory infection:
- Acute pharyngitis
- acute ear infection
- Catch cold
Causes of lower respiratory infection:
- Bronchitis
- Pneumonia
- bronchiolitis
Who is at risk for acute respiratory infection?
Viruses and bacteria are almost impossible to avoid, but certain risk factors increase the chances of developing acute respiratory infections.
The immune systems of children and the elderly are more susceptible to being affected by viruses.
Children are especially at risk because of their constant contact with other children who could be carriers of viruses. Children often do not wash their hands regularly in daily life. They are also more likely to rub their eyes and put their fingers in their mouths, which leads to the spread of viruses.
People with heart disease or other lung problems are more likely to develop acute respiratory infections. Anyone whose immune system is weakened by another disease is at risk. Smokers are also at higher risk and have greater recovery problems.
How is acute respiratory infection diagnosed?
In a respiratory examination, the doctor focuses on your breathing. They will check for the fluid and inflammation in the lungs by listening for the abnormal sounds in your lungs when you breathe. The doctor may look at your nose and ears and examine your throat.
If your doctor thinks the infection is in the lower respiratory tract, an X-ray or CT scan to check the condition of the lungs may be necessary.
Pulmonary function tests have been useful as diagnostic tools. A pulse oximeter, also known as a pulse oximeter, can check the amount of oxygen reaching the lungs. The doctor may also take a swab from your nose or mouth, or ask you to cough up a sample of sputum (material coughed up from the lungs) to check for the type of virus or bacteria causing the illness.
How is acute respiratory infection treated?
With so many viruses, there are no known cures. Your doctor may prescribe medications to control your symptoms while monitoring your condition. If your doctor suspects you may have a bacterial infection, he or she may prescribe antibiotics.
The possible complications of the acute respiratory infection
Complications of acute respiratory infection are very serious and can lead to permanent damage and even death. They include:
- respiratory arrest, which occurs when the lungs stop working
- Respiratory failure, a rise in carbon dioxide in the blood because your lungs are not working properly
- congestive heart failure
- Prevent acute respiratory infections
Most causes of acute respiratory infection cannot be cured. Therefore, prevention is the best way to ward off harmful respiratory infections.
Getting the MMR (measles, mumps, and rubella) and whooping cough vaccine will greatly reduce your risk of developing a respiratory infection. You may also benefit from the flu shot and pneumothorax.
Practice good health habits:
- Wash your hands frequently, especially after you have been in the public place.
- Always sneeze into the arm of your shirt or into a tissue. Although this may not relieve your symptoms, it will prevent you from spreading infectious diseases.
- Avoid touching your face, especially your eyes and the mouth, to prevent germs from entering your system.
You should also avoid smoking and make sure to include plenty of vitamins in your diet, such as vitamin C, which helps boost your immune system. Vitamin C is retained in immune cells, and vitamin C deficiency has been linked to an increased susceptibility to infections. While the research is unclear whether vitamin C can prevent acute respiratory infections, there is evidence that it can shorten the duration and/or severity of some infections.
What causes acute upper respiratory infection?
Both viruses and bacteria can cause severe URIs:
- Viruses
- flu
- glandular
- coxsackie virus
- parainfluenza virus
- respiratory syncytial virus
- human kinetic virus
- bacteria
- Group A beta-hemolytic streptococci
- Group C beta-hemolytic streptococci
- Corynebacterium diphtheria
- Neisseria gonorrhea (gonorrhea)
- Pulmonary chlamydia (chlamydia)
What are the types of the acute upper respiratory infection?
The types of URIs refer to the parts of the upper respiratory tract most closely associated with infection. In addition to the common cold, there are other types of the URIs:
1. Sinusitis
Sinusitis is an inflammation of the sinuses.
2. Epiglottitis
Epiglottitis is inflammation of the epiglottis, the upper part of the windpipe. It protects the airway from foreign particles that can enter the lungs. Swelling of the epiglottis is dangerous because it can block airflow into the windpipe.
3. Laryngitis
Laryngitis is an inflammation of the larynx or larynx.
4. Bronchitis
Bronchitis is inflammation of the airways. The left and right bronchi branch off from the trachea and pass to the right and left lungs.
BY: Web Team
Magazine
COMMENTS: No Comments
 01 Apr 2022
01 Apr 2022
10 Reasons Why Physiotherapy is Beneficial
Physical therapy helps people of all ages with medical conditions, illnesses, or injuries that limit their regular ability to move and function.
A customized physical therapy program can help individuals return to their previous level of functioning, and encourage activities and lifestyle changes that can help prevent further injury and improve overall health and well-being. Primary care physicians often refer patients to physical therapy at the first sign of a problem, since it is considered a conservative approach to problem management. Wondering what makes physical therapy so important? In honor of Physical Therapy Month in October, here are 10 ways it might help you:

1. Reducing or eliminating pain
Therapeutic exercises and the manual therapy techniques such as moving joints and the soft tissues, or treatments such as ultrasound, tape or electrical stimulation can help relieve pain and restore muscle and joint function to reduce pain. Such treatments can also prevent the pain from returning.
2. Avoid surgery
If physical therapy helps relieve pain or recover from an injury, surgery may not be needed. And even if surgery is required, you may benefit from preoperative physical therapy. If you are to have stronger surgery and are in better shape, you will recover faster after that in many cases. Also, by avoiding surgery, healthcare costs are reduced.
3. Improve mobility
If you have difficulty standing, walking or moving — no matter your age — physical therapy can help. Stretching and strengthening exercises help to restore your mobility. Physical therapists can fit individuals properly using a cane, crutches, or other assistive device, or evaluate orthotic prescription. By customizing an individualized care plan, any activity important to an individual’s life can be practiced and adapted to ensure maximum performance and safety.
4. Stroke recovery
It is common to lose some degree of the function and movement after a stroke. Physical therapy helps strengthen weak parts of the body and improve walking and balance. Physical therapists can also improve stroke patients’ ability to move around in bed so they can be more independent at home, and reduce their burden of care for toileting.
5. Recovering from or preventing a sports injury
Physical therapists understand how different sports can increase your risk of certain types of injuries (such as stress fractures for distance runners). They can design appropriate recovery or prevention programs for you to ensure a safe return to your sport.
6. It improves your balance and prevents falls
When you begin physical therapy, you will be screened for your risk of falling. If you are at high risk of falling, therapists will provide exercises that safely and carefully challenge your balance as a way to mimic real-life situations. Therapists also help you with exercises to improve coordination and assistive devices to aid in safe walking. When a balance problem is caused by a problem with the vestibular system, physiotherapists can perform specific maneuvers that can quickly restore proper vestibular functioning, and reduce and eliminate symptoms of dizziness or lightheadedness.
7. Management of diabetes and vascular disease
As part of a comprehensive diabetes management plan, exercise can help effectively control your blood sugar. In addition, people with the diabetes may have problems with sensation in their feet and legs. Physical therapists can help provide and educate these patients about proper foot care to prevent further problems in the future.
8. Managing age issues
As individuals age, they may develop arthritis, osteoarthritis, or need a joint replacement. Physical therapists are experts in helping patients recover from joint replacement, and conservatively managing cases of arthritis or osteoarthritis.
9. Heart and lung disease management
While patients may complete cardiac rehabilitation after a heart attack or procedure, you may also receive physical therapy if your daily functioning is affected. For lung problems, physical therapy can improve quality of life with strengthening, conditioning, and breathing exercises, and by helping patient’s clear fluid in the lungs.
10. Managing Women’s Health and Other Conditions
Women have the specific health concerns, such as pregnancy and postpartum care. Physical therapists can provide specialized management of issues related to women’s health. In addition, PT can provide specialized treatment for: Bowel Incontinence, Breast Cancer, Constipation, Fibromyalgia, Lymphedema, Male Pelvic Health, Pelvic Pain, and Urinary Incontinence.
BY: Web Team
Magazine
COMMENTS: No Comments
 01 Apr 2022
01 Apr 2022
How can physical therapy help?
In physical therapy, also known as the PT, trained professionals evaluate and the treat abnormal physical function related to an injury, disability, or other health condition.
According to the American Physical Therapy Association, physical therapists are trained and licensed movement experts. They can diagnose and treat a range of the injuries, disabilities, and health conditions.

Physical therapists aim to improve a person’s range of motion, quality of life, and prevent further injury or disability.
Licensed physical therapists work in a range of health care settings, including outpatient offices, private clinics, hospitals, rehabilitation centers, nursing homes, home health, sports and fitness settings, schools, nursing homes, professional settings, government agencies, and research centers.
What are you expecting?
A physical therapist assists in patient care at all stages of recovery, from initial diagnosis to the restorative and preventive stages of recovery. Physical therapy may be a stand-alone option, or it may support other treatments.
Some patients are referred by a doctor to a physical therapist, while others seek treatment on their own.
According to the World Federation of Physiotherapy, a physical therapist receives training that enables them to:
- Perform a physical examination and assessment of the person’s movement, flexibility, muscle and joint movement and performance, including knowledge of their health history
- Giving clinical diagnosis, prognosis and plan of care with short and long-term goals
- Carry out treatment and physiotherapy intervention
- Make recommendations for self-management, including exercises that anyone can do at home
Aside from physical manipulation, physical therapy may include:
1. Iontophoresis
This electrical current is used to deliver certain medications, such as topical steroids. This can reduce the presence of inflammation.
2. Electrical stimulation (e-stim)
There are two types of electrical stimulation. Transcutaneous electrical nerve stimulation (TENS) reduces pain. By contrast, neuromuscular electrical stimulation stimulates muscular motor units to improve muscle engagement.
3. Heat, moist heat, and cold therapy
These may provide benefits for a range of conditions.
4. Light therapy
This involves using the special lights and lasers to treat certain medical conditions.
5. Physiotherapy may help in common cases
Physical therapists can provide complementary treatment for a variety of medical conditions, depending on their specialty.
Although physical therapists may not directly and independently treat a medical condition other than purely musculoskeletal conditions, they work to improve recovery or educate the person about how to improve their movement patterns.
Some of the conditions that can benefit from physical therapy are:
- Cardiopulmonary conditions, such as chronic obstructive pulmonary disease, cystic fibrosis, and heart failure following myocardial infarction
- Conditions that affect the hand, such as the carpal tunnel syndrome and trigger finger
- Musculoskeletal dysfunction, including back pain, rotator cuff tear, and temporomandibular joint disorders
- Neurological conditions, such as stroke, spinal cord injury, Parkinson’s disease, multiple sclerosis, vestibular dysfunction, and traumatic brain injury
- Pediatric diseases, including cerebral palsy and muscular dystrophy
- Sports injuries, such as concussion and tennis elbow
- Poor female and pelvic floor health, including enuresis and lymphedema
- Skin diseases or injuries, such as burns, wound care, and diabetic ulcers
Benefits of physical therapy
Depending on the reason for the treatment, the benefits of physical therapy may include:
- Pain management with reduced need for opioids
- Avoid surgery
- Improve movement and movement
- Healing from injury or trauma
- Recovery from stroke or paralysis
- Fall prevention
- improve balance
- Managing age-related medical problems
A sports therapist can help an athlete achieve maximum performance by strengthening specific parts of the body and using muscles in new ways.
A physical therapist or other health care professional can advise individuals about the benefits of their personal medical history and their need for treatment.
Species
There are many types of physical therapy, and therapists usually choose a specialty. These types include:
1. Orthopedic physical therapy
treats musculoskeletal injuries, including the muscles, bones, ligaments, fascia, and tendons. They are suitable for conditions such as fractures, sprains, tendinitis, bursitis, chronic health problems, and rehabilitation or recovery from orthopedic surgery. Patients may undergo treatment with joint movement, manual therapy, strength exercises, movement training, and other methods.
2. Physical therapy for seniors
It can help seniors with conditions that affect their movement and physical function, including arthritis, osteoporosis, Alzheimer’s disease, hip and joint replacement, balance disorders, and incontinence. This type of intervention aims to restore mobility, reduce pain, and increase fitness levels.
3. Neurophysiotherapy
It can help people with neurological conditions, such as Alzheimer’s disease, brain injury, cerebral palsy, multiple sclerosis, Parkinson’s disease, spinal cord injury, and stroke. Treatment may aim to increase limb response, improve movement patterns, manage tone, improve strength, and enhance balance.
4. Cardiovascular and pulmonary rehabilitation
This can benefit people affected by certain cardiopulmonary diseases and surgical procedures. Treatment can increase muscular and cardiovascular endurance and endurance.
5. Wound care therapy
This can help ensure that a fused wound receives enough oxygen and blood by improving circulation. Physical therapy may include the use of manual therapies, electronic stimulation, acupressure, and wound care.
6. Vestibular therapy
aims to treat balance problems that can result from diseases of the inner ear. Vestibular physical therapy includes a number of exercises and manual techniques that can help patients restore their balance and coordination.
7. Decongestant therapy
It can help drain accumulated fluid in patients with lymphedema and other conditions involving fluid buildup.
8. Pelvic floor rehabilitation
This can help treat conditions that affect the pelvic floor, such as urinary or fecal incontinence, urinary urgency and pelvic pain as a result of injuries, surgery, or due to certain conditions.
BY: Web Team
Magazine
COMMENTS: No Comments
 31 Mar 2022
31 Mar 2022
Fatty liver disease
The fatty liver disease is a common condition caused by the storage of excess fat in the liver. Most people have no symptoms and it does not cause the serious problems. However, in some cases, it can lead to liver damage. The good news is that you can often prevent or even reverse fatty liver disease through lifestyle changes.

What is fatty liver disease?
Fatty liver disease (steatosis) is a common condition caused by the buildup of too much fat in the liver. A healthy liver contains the small amount of fat. It becomes a problem when fat reaches 5% to 10% of the liver’s weight.
Why is fatty liver disease bad?
In most cases, fatty liver disease does not cause any serious problems or prevent the liver from working normally. But for 7% to 30% of people with this condition, the fatty liver disease gets worse over time. It progresses through three stages:
- The liver becomes inflamed (swollen), damaging its tissues. This stage is called steatohepatitis.
- Scar tissue forms where the liver is damaged. This process is called fibrosis.
- Extensive scar tissue replaces healthy tissue. At this point, you have cirrhosis.
Cirrhosis
Cirrhosis is caused by severe damage to the liver. Hard scar tissue that replaces healthy liver tissue slows down the functioning of the liver. Ultimately, it can completely hamper liver function. Cirrhosis can lead to liver failure and the liver cancer.
What are the forms of fatty liver disease?
There are two main types of the fatty liver disease:
1. Alcoholic liver disease
Alcoholic fatty liver is the buildup of the fat in the liver as a result of excessive alcohol consumption. (Moderate drinking is defined as one drink per day for women and up to two drinks per day for men.) About 5% of people in the United States have this type of liver disease.
2. Non-alcoholic fatty liver disease
Nonalcoholic fatty liver disease affects people who don’t drink a lot. The condition affects one in three adults and one in the 10 children in the United States. Researchers have not found the exact cause of the nonalcoholic fatty liver disease. Several factors, such as the obesity and the diabetes, can increase your risk.
Who gets fatty liver disease?
You have a higher chance of developing fatty liver disease if you:
- They are of Hispanic or Asian descent.
- You are a postmenopausal woman (a woman whose periods have stopped).
- You are obese with a high percentage of belly fat.
- You suffer from the high blood pressure, diabetes or the high cholesterol.
- You have obstructive sleep apnea (a blocked airway that causes breathing to stop and start during sleep).
What causes fatty liver disease?
Some people develop the fatty liver disease without having any preexisting conditions. But these risk factors make you more likely to get it:
- Obesity or being overweight.
- Having type 2 diabetes or insulin resistance.
- The Metabolic syndrome (insulin resistance, high blood pressure, high cholesterol and high triglyceride levels).
- Take certain prescription medications, such as amiodarone (Cordarone), diltiazem (Cardizem), tamoxifen (Nolvadex®), or steroids.
What are the symptoms of fatty liver disease?
People with the fatty liver disease often have no symptoms until the disease progresses to cirrhosis. If you have symptoms, they may also include:
- Abdominal pain or a feeling of fullness in the upper right side of the tummy (abdomen).
- Nausea, loss of appetite or weight loss.
- Yellowing of the skin and the whites of the eyes.
- Flatulence of the abdomen and legs (edema).
- Extreme tiredness or mental confusion.
How is fatty liver disease treated?
There is no specific medication for fatty liver disease. Instead, doctors focus on helping you control the factors that contribute to this condition. They also recommend making the lifestyle changes that can significantly improve your health. Treatment includes:
- Avoid alcohol.
- Lose weight.
- Take medications to control diabetes, cholesterol, and triglycerides (fats in the blood).
- Take vitamin E and thiazolidinedione’s (medicines used to treat diabetes such as Actos® and Avandia®) for certain conditions.
How can fatty liver disease be prevented?
The best way to avoid the fatty liver disease is to do the things that maintain overall health:
- Maintain a healthy weight. If you are overweight or the obese, lose weight gradually.
- I exercise regularly.
- Reduce your alcohol consumption.
- Take medications as prescribed.
Can fatty liver disease be treated?
If you avoid alcohol or lose weight, it is possible to reduce liver fat and inflammation and reverse early liver damage.
Will Fatty Liver Disease Kill You?
Fatty liver disease does not cause major problems for most people. However, it can turn into a more serious problem if it develops into cirrhosis. Untreated cirrhosis eventually leads to liver failure or liver cancer. Your liver is the organ you cannot live without.
What is a good diet for fatty liver?
Eat a balanced diet to lose weight slowly but surely. The rapid weight loss can actually worsen the fatty liver disease. Doctors often recommend the Mediterranean diet, which is the high in vegetables, fruits, and good fats. Ask your doctor or dietitian for advice on healthy approaches to losing weight.
- What questions should I ask my doctor?
- Am I taking any medications that can contribute to fatty liver disease?
- How much damage to the liver?
- How long will it take to reverse liver damage?
- What is a healthy weight for me?
- Can I talk to a dietitian or go to classes to learn about healthy eating?
- How can I get the treatment for alcohol use disorder?
Note from Thumbay University Hospital
Keep in mind that fatty liver disease is an early warning sign to help you avoid potentially fatal liver disease, such as cirrhosis or liver cancer. Even if you do not have symptoms or any problems with liver function at this point, it is still important to take steps to stop or reverse your fatty liver disease.
BY: Web Team
Magazine
COMMENTS: No Comments